Abstract
Introduction
intra-abdominal candidiasis (IAC) may include Candida involvement of peritoneum or intra-abdominal abscess and is burdened by high morbidity and mortality rates in surgical patients. Unfortunately, international guidelines do not specifically address this particular clinical setting due to heterogeneity of definitions and scant direct evidence. In order to cover this unmet clinical need, the Italian Society of Intensive Care and the International Society of Chemotherapy endorsed a project aimed at producing practice recommendations for the management of immune-competent adult patients with IAC.
Methods
A multidisciplinary expert panel of 22 members (surgeons, infectious disease and intensive care physicians) was convened and assisted by a methodologist between April 2012 and May 2013. Evidence supporting each statement was graded according to the European Society of Clinical Microbiology and Infection Diseases (ESCMID) grading system.
Results
Only a few of the numerous recommendations can be summarized in the Abstract. Direct microscopy examination for yeast detection from purulent and necrotic intra-abdominal specimens during surgery or by percutaneous aspiration is recommended in all patients with nonappendicular abdominal infections including secondary and tertiary peritonitis. Samples obtained from drainage tubes are not valuable except for evaluation of colonization. Prophylactic usage of fluconazole should be adopted in patients with recent abdominal surgery and recurrent gastrointestinal perforation or anastomotic leakage. Empirical antifungal treatment with echinocandins or lipid formulations of amphotericin B should be strongly considered in critically ill patients or those with previous exposure to azoles and suspected intra-abdominal infection with at least one specific risk factor for Candida infection. In patients with nonspecific risk factors, a positive mannan/antimannan or (1→3)-β-d-glucan (BDG) or polymerase chain reaction (PCR) test result should be present to start empirical therapy. Fluconazole can be adopted for the empirical and targeted therapy of non-critically ill patients without previous exposure to azoles unless they are known to be colonized with a Candida strain with reduced susceptibility to azoles. Treatment can be simplified by stepping down to an azole (fluconazole or voriconazole) after at least 5–7 days of treatment with echinocandins or lipid formulations of amphotericin B, if the species is susceptible and the patient has clinically improved.
Conclusions
Specific recommendations were elaborated on IAC management based on the best direct and indirect evidence and on the expertise of a multinational panel.
Similar content being viewed by others
Abbreviations
- SITI:
-
Italian Society of Intensive Care
- ISC:
-
International Society of Chemotherapy
- ESCMID:
-
European Society of Clinical Microbiology and Infectious Diseases
- EP:
-
Expert panel
- GI:
-
Gastrointestinal
- IAC:
-
intra-abdominal candidiasis
- ICU:
-
Intensive care unit
- CLSI:
-
Clinical and Laboratory Standards Institute
- EUCAST:
-
European Committee on Antimicrobial Susceptibility Testing
- CAGTA:
-
C. albicans germ tube antibodies
- BDG:
-
(1→3)-β-d-Glucan
- IDSA:
-
Infectious Diseases Society of America
- CNS:
-
Central nervous system
References
Dupont H, Paugam-Burtz C, Muller-Serieys C, Fierobe L, Chosidow D, Marmuse JP, Mantz J, Desmonts JM (2002) Predictive factors of mortality due to polymicrobial peritonitis with Candida isolation in peritoneal fluid in critically ill patients. Arch Surg 137(12):1341–1346
Sandven P, Qvist H, Skovlund E, Giercksky KE (2002) Significance of Candida recovered from intraoperative specimens in patients with intra-abdominal perforations. Crit Care Med 30(3):541–547
Montravers P, Dupont H, Gauzit R, Veber B, Auboyer C, Blin P, Hennequin C, Martin C (2006) Candida as a risk factor for mortality in peritonitis. Crit Care Med 34(3):646–652
Montravers P, Mira JP, Gangneux JP, Leroy O, Lortholary O (2011) A multicentre study of antifungal strategies and outcome of Candida spp. peritonitis in intensive-care units. Clin Microbiol Infect 17(7):1061–1067
Ullmann AJ, Akova M, Herbrecht R, Viscoli C, Arendrup MC, Arikan-Akdagli S, Bassetti M, Bille J, Calandra T, Castagnola E et al (2012) ESCMID* guideline for the diagnosis and management of Candida diseases 2012: adults with haematological malignancies and after haematopoietic stem cell transplantation (HCT). Clin Microbiol Infect 18(Suppl 7):53–67
Ruhnke M, Rickerts V, Cornely OA, Buchheidt D, Glockner A, Heinz W, Hohl R, Horre R, Karthaus M, Kujath P et al (2011) Diagnosis and therapy of Candida infections: joint recommendations of the German Speaking Mycological Society and the Paul-Ehrlich-Society for Chemotherapy. Mycoses 54(4):279–310
Pappas PG, Kauffman CA, Andes D, Benjamin DK Jr, Calandra TF, Edwards JE Jr, Filler SG, Fisher JF, Kullberg BJ, Ostrosky-Zeichner L et al (2009) Clinical practice guidelines for the management of candidiasis: 2009 update by the Infectious Diseases Society of America. Clin Infect Dis 48(5):503–535
Aguado JM, Ruiz-Camps I, Munoz P, Mensa J, Almirante B, Vazquez L, Rovira M, Martin-Davila P, Moreno A, Alvarez-Lerma F et al (2011) Guidelines for the treatment of invasive candidiasis and other yeasts. Spanish Society of Infectious Diseases and Clinical Microbiology (SEIMC). 2010 Update. Enferm Infecc Microbiol Clin 29(5):345–361
Loblaw DA, Prestrud AA, Somerfield MR, Oliver TK, Brouwers MC, Nam RK, Lyman GH, Basch E (2012) American Society of Clinical Oncology Clinical Practice Guidelines: formal systematic review-based consensus methodology. J Clin Oncol 30(25):3136–3140
Girmenia C, Barosi G, Aversa F, Bacigalupo A, Barbui T, Baronciani D, Bosi A, Candoni A, Locasciulli A, Locatelli F et al (2009) Prophylaxis and treatment of invasive fungal diseases in allogeneic stem cell transplantation: results of a consensus process by Gruppo Italiano Trapianto di Midollo Osseo (GITMO). Clin Infect Dis 49(8):1226–1236
Kullberg BJ, Verweij PE, Akova M, Arendrup MC, Bille J, Calandra T, Cuenca-Estrella M, Herbrecht R, Jacobs F, Kalin M et al (2011) European expert opinion on the management of invasive candidiasis in adults. Clin Microbiol Infect 17(Suppl 5):1–12
Murphy MK, Black NA, Lamping DL, McKee CM, Sanderson CF, Askham J, Marteau T (1998) Consensus development methods, and their use in clinical guideline development. Health Technol Assess 2(3):i–iv 1–88
Lamme B, Van Ruler O, Boermeester MA (2002) Surgical re-intervention in postoperative peritonitis based on longitudinal scoring systems. Intensive Care Med 28(11):1673 author reply 1674
Blot SI, Vandewoude KH, De Waele JJ (2007) Candida peritonitis. Curr Opin Crit Care 13(2):195–199
Maggard MA, McGory ML, Ko CY (2006) Development of quality indicators: lessons learned in bariatric surgery. Am Surg 72(10):870–874
Cornely OA, Bassetti M, Calandra T, Garbino J, Kullberg BJ, Lortholary O, Meersseman W, Akova M, Arendrup MC, Arikan-Akdagli S et al (2012) ESCMID* guideline for the diagnosis and management of Candida diseases 2012: non-neutropenic adult patients. Clin Microbiol Infect 18(Suppl 7):19–37
de Ruiter J, Weel J, Manusama E, Kingma WP, van der Voort PH (2009) The epidemiology of intra-abdominal flora in critically ill patients with secondary and tertiary abdominal sepsis. Infection 37(6):522–527
Lee SC, Fung CP, Chen HY, Li CT, Jwo SC, Hung YB, See LC, Liao HC, Loke SS, Wang FL et al (2002) Candida peritonitis due to peptic ulcer perforation: incidence rate, risk factors, prognosis and susceptibility to fluconazole and amphotericin B. Diagn Microbiol Infect Dis 44(1):23–27
Ostrosky-Zeichner L (2003) New approaches to the risk of Candida in the intensive care unit. Curr Opin Infect Dis 16(6):533–537
Dupont H, Bourichon A, Paugam-Burtz C, Mantz J, Desmonts JM (2003) Can yeast isolation in peritoneal fluid be predicted in intensive care unit patients with peritonitis? Crit Care Med 31(3):752–757
Pittet D, Monod M, Suter PM, Frenk E, Auckenthaler R (1994) Candida colonization and subsequent infections in critically ill surgical patients. Ann Surg 220(6):751–758
Leon C, Ruiz-Santana S, Saavedra P, Galvan B, Blanco A, Castro C, Balasini C, Utande-Vazquez A, de Gonzalez Molina FJ, Blasco-Navalproto MA et al (2009) Usefulness of the “Candida score” for discriminating between Candida colonization and invasive candidiasis in non-neutropenic critically ill patients: a prospective multicenter study. Crit Care Med 37(5):1624–1633
Leon C, Ruiz-Santana S, Saavedra P, Almirante B, Nolla-Salas J, Alvarez-Lerma F, Garnacho-Montero J, Leon MA (2006) A bedside scoring system (“Candida score”) for early antifungal treatment in nonneutropenic critically ill patients with Candida colonization. Crit Care Med 34(3):730–737
Tapia GG, Razonable RR, Eckel-Passow JE, Lahr BD, Afessa B, Keegan MT, Catania J, Baddour LM (2012) A scoring model of factors associated with Candida glabrata candidemia among critically ill patients. Mycoses 55(3):228–236
Playford EG, Webster AC, Sorrell TC, Craig JC (2006) Systematic review and meta-analysis of antifungal agents for preventing fungal infections in liver transplant recipients. Eur J Clin Microbiol Infect Dis 25(9):549–561
Chow JK, Golan Y, Ruthazer R, Karchmer AW, Carmeli Y, Lichtenberg D, Chawla V, Young J, Hadley S (2008) Factors associated with candidemia caused by non-albicans Candida species versus Candida albicans in the intensive care unit. Clin Infect Dis 46(8):1206–1213
Chi HW, Yang YS, Shang ST, Chen KH, Yeh KM, Chang FY, Lin JC (2011) Candida albicans versus non-albicans bloodstream infections: the comparison of risk factors and outcome. J Microbiol Immunol Infect 44(5):369–375
Garnacho-Montero J, Diaz-Martin A, Garcia-Cabrera E, de Ruiz Perez Pipaon M, Hernandez-Caballero C, Aznar-Martin J, Cisneros JM, Ortiz-Leyba C (2010) Risk factors for fluconazole-resistant candidemia. Antimicrob Agents Chemother 54(8):3149–3154
Tumbarello M, Caldarola G, Tacconelli E, Morace G, Posteraro B, Cauda R, Ortona L (1996) Analysis of the risk factors associated with the emergence of azole resistant oral candidosis in the course of HIV infection. J Antimicrob Chemother 38(4):691–699
Magill SS, Shields C, Sears CL, Choti M, Merz WG (2006) Triazole cross-resistance among Candida spp.: case report, occurrence among bloodstream isolates, and implications for antifungal therapy. J Clin Microbiol 44(2):529–535
Pfaller MA, Diekema DJ (2004) Twelve years of fluconazole in clinical practice: global trends in species distribution and fluconazole susceptibility of bloodstream isolates of Candida. Clin Microbiol Infect 10(Suppl 1):11–23
Montravers P, Gauzit R, Muller C, Marmuse JP, Fichelle A, Desmonts JM (1996) Emergence of antibiotic-resistant bacteria in cases of peritonitis after intraabdominal surgery affects the efficacy of empirical antimicrobial therapy. Clin Infect Dis 23(3):486–494
Manolakaki D, Velmahos G, Kourkoumpetis T, Chang Y, Alam HB, De Moya MM, Mylonakis E (2010) Candida infection and colonization among trauma patients. Virulence 1(5):367–375
Calandra T, Bille J, Schneider R, Mosimann F, Francioli P (1989) Clinical significance of Candida isolated from peritoneum in surgical patients. Lancet 2(8677):1437–1440
Piarroux R, Grenouillet F, Balvay P, Tran V, Blasco G, Millon L, Boillot A (2004) Assessment of preemptive treatment to prevent severe candidiasis in critically ill surgical patients. Crit Care Med 32(12):2443–2449
Chiarini A, Palmeri A, Amato T, Immordino R, Distefano S, Giammanco A (2008) Detection of bacterial and yeast species with the Bactec 9120 automated system with routine use of aerobic, anaerobic, and fungal media. J Clin Microbiol 46(12):4029–4033
Pfaller MA, Diekema DJ, Sheehan DJ (2006) Interpretive breakpoints for fluconazole and Candida revisited: a blueprint for the future of antifungal susceptibility testing. Clin Microbiol Rev 19(2):435–447
Leroy O, Mira JP, Montravers P, Gangneux JP, Gouin F, Sollet JP, Carlet J, Reynes J, Rosenheim M, Regnier B et al (2008) Invasive candidiasis in ICU: analysis of antifungal treatments in the French study AmarCand. Ann Fr Anesth Reanim 27(12):999–1007
Clinical Laboratory Standards Institute (2012) Reference method for broth dilution antifungal susceptibility testing for yeasts. Fourth Informational Supplement. CLSI document M27-S4. Clinical and Laboratory Standards Institute, Wayne
European Committee on Antimicrobial Susceptibility Testing 2013. Breakpoint tables for interpretation of MICs Version 6.1
Rex JH, Pfaller MA, Walsh TJ, Chaturvedi V, Espinel-Ingroff A, Ghannoum MA, Gosey LL, Odds FC, Rinaldi MG, Sheehan DJ et al (2001) Antifungal susceptibility testing: practical aspects and current challenges. Clin Microbiol Rev 14(4):643–658 table of contents
Prakash A, Sharma D, Saxena A, Somashekar U, Khare N, Mishra A, Anvikar A (2008) Effect of Candida infection on outcome in patients with perforation peritonitis. Indian J Gastroenterol 27(3):107–109
Cortes JA, Concha MA, Cediel TL, Castillo JS (2011) Diagnostic methods in candidemia: a systematic review of literature with meta-analysis. Rev Chilena Infectol 28(5):423–428
Lu Y, Chen YQ, Guo YL, Qin SM, Wu C, Wang K (2011) Diagnosis of invasive fungal disease using serum (1–>3)-beta-d-glucan: a bivariate meta-analysis. Intern Med 50(22):2783–2791
Tissot F, Lamoth F, Hauser PM, Orasch C, Fluckiger U, Siegemund, Zimmerli S, Calandra T, Bille J, Eggimann P et al (2013) Beta-glucan antigenemia anticipates diagnosis of blood culture-negative intra-abdominal candidiasis. Am J Respir Crit Care Med
Nguyen MH, Wissel MC, Shields RK, Salomoni MA, Hao B, Press EG, Shields RM, Cheng S, Mitsani D, Vadnerkar A et al (2012) Performance of Candida real-time polymerase chain reaction, beta-d-glucan assay, and blood cultures in the diagnosis of invasive candidiasis. Clin Infect Dis 54(9):1240–1248
Sendid B, Tabouret M, Poirot JL, Mathieu D, Fruit J, Poulain D (1999) New enzyme immunoassays for sensitive detection of circulating Candida albicans mannan and antimannan antibodies: useful combined test for diagnosis of systemic candidiasis. J Clin Microbiol 37(5):1510–1517
Sendid B, Poirot JL, Tabouret M, Bonnin A, Caillot D, Camus D, Poulain D (2002) Combined detection of mannanaemia and antimannan antibodies as a strategy for the diagnosis of systemic infection caused by pathogenic Candida species. J Med Microbiol 51(5):433–442
Sendid B, Jouault T, Coudriau R, Camus D, Odds F, Tabouret M, Poulain D (2004) Increased sensitivity of mannanemia detection tests by joint detection of alpha- and beta-linked oligomannosides during experimental and human systemic candidiasis. J Clin Microbiol 42(1):164–171
Yera H, Sendid B, Francois N, Camus D, Poulain D (2001) Contribution of serological tests and blood culture to the early diagnosis of systemic candidiasis. Eur J Clin Microbiol Infect Dis 20(12):864–870
Sendid B, Dotan N, Nseir S, Savaux C, Vandewalle P, Standaert A, Zerimech F, Guery BP, Dukler A, Colombel JF et al (2008) Antibodies against glucan, chitin, and Saccharomyces cerevisiae mannan as new biomarkers of Candida albicans infection that complement tests based on C. albicans mannan. Clin Vaccine Immunol 15(12):1868–1877
Pickering JW, Sant HW, Bowles CA, Roberts WL, Woods GL (2005) Evaluation of a (1>3)-beta-d-glucan assay for diagnosis of invasive fungal infections. J Clin Microbiol 43(12):5957–5962
Del Bono V, Delfino E, Furfaro E, Mikulska M, Nicco E, Bruzzi P, Mularoni A, Bassetti M, Viscoli C (2011) Clinical performance of the (1,3)-beta-d-glucan assay in early diagnosis of nosocomial Candida bloodstream infections. Clin Vaccine Immunol 18(12):2113–2117
Bille J (2010) New nonculture-based methods for the diagnosis of invasive candidiasis. Curr Opin Crit Care 16(5):460–464
Avni T, Leibovici L, Paul M (2011) PCR diagnosis of invasive candidiasis: systematic review and meta-analysis. J Clin Microbiol 49(2):665–670
van Veen SQ, Claas EC, Kuijper EJ (2010) High-throughput identification of bacteria and yeast by matrix-assisted laser desorption ionization-time of flight mass spectrometry in conventional medical microbiology laboratories. J Clin Microbiol 48(3):900–907
Ibelings MS, Maquelin K, Endtz HP, Bruining HA, Puppels GJ (2005) Rapid identification of Candida spp. in peritonitis patients by Raman spectroscopy. Clin Microbiol Infect 11(5):353–358
Eggimann P, Francioli P, Bille J, Schneider R, Wu MM, Chapuis G, Chiolero R, Pannatier A, Schilling J, Geroulanos S et al (1999) Fluconazole prophylaxis prevents intra-abdominal candidiasis in high-risk surgical patients. Crit Care Med 27(6):1066–1072
Senn L, Eggimann P, Ksontini R, Pascual A, Demartines N, Bille J, Calandra T, Marchetti O (2009) Caspofungin for prevention of intra-abdominal candidiasis in high-risk surgical patients. Intensive Care Med 35(5):903–908
Khoury W, Szold O, Soffer D, Kariv Y, Wasserlauf R, Klausner JM, Ogorek D, Weinbroum AA (2010) Prophylactic fluconazole does not improve outcome in patients with purulent and fecal peritonitis due to lower gastrointestinal perforation. Am Surg 76(2):197–202
Posteraro B, De Pascale G, Tumbarello M, Torelli R, Pennisi MA, Bello G, Maviglia R, Fadda G, Sanguinetti M, Antonelli M (2011) Early diagnosis of candidemia in intensive care unit patients with sepsis: a prospective comparison of (1–>3)-beta-d-glucan assay, Candida score, and colonization index. Crit Care 15(5):R249
Cruciani M, de Lalla F, Mengoli C (2005) Prophylaxis of Candida infections in adult trauma and surgical intensive care patients: a systematic review and meta-analysis. Intensive Care Med 31(11):1479–1487
Vardakas KZ, Samonis G, Michalopoulos A, Soteriades ES, Falagas ME (2006) Antifungal prophylaxis with azoles in high-risk, surgical intensive care unit patients: a meta-analysis of randomized, placebo-controlled trials. Crit Care Med 34(4):1216–1224
Shorr AF, Chung K, Jackson WL, Waterman PE, Kollef MH (2005) Fluconazole prophylaxis in critically ill surgical patients: a meta-analysis. Crit Care Med 33(9):1928–1935 quiz 1936
Shan YS, Sy ED, Wang ST, Lee JC, Lin PW (2006) Early presumptive therapy with fluconazole for occult Candida infection after gastrointestinal surgery. World J Surg 30(1):119–126
Agvald-Ohman C, Klingspor L, Hjelmqvist H, Edlund C (2008) Invasive candidiasis in long-term patients at a multidisciplinary intensive care unit: Candida colonization index, risk factors, treatment and outcome. Scand J Infect Dis 40(2):145–153
Gafter-Gvili A, Vidal L, Goldberg E, Leibovici L, Paul M (2008) Treatment of invasive candidal infections: systematic review and meta-analysis. Mayo Clin Proc 83(9):1011–1021
Kujath P, Lerch K, Kochendorfer P, Boos C (1993) Comparative study of the efficacy of fluconazole versus amphotericin B/flucytosine in surgical patients with systemic mycoses. Infection 21(6):376–382
Golan Y, Wolf MP, Pauker SG, Wong JB, Hadley S (2005) Empirical anti-Candida therapy among selected patients in the intensive care unit: a cost-effectiveness analysis. Ann Intern Med 143(12):857–869
Chen Q, Lin MH, Chen ML, Liu ZY, Chai D, Wang R (2012) Efficacy and safety of micafungin for invasive candida infections: a meta-analysis of randomized controlled trials. Chin Med J (Engl) 125(2):345–351
Pea F, Viale P, Furlanut M (2005) Antimicrobial therapy in critically ill patients: a review of pathophysiological conditions responsible for altered disposition and pharmacokinetic variability. Clin Pharmacokinet 44(10):1009–1034
Romani L (2012) Amphotericin B still in the headlines. Pathog Glob Health 106(2):80–81
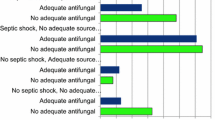
Kollef M, Micek S, Hampton N, Doherty JA, Kumar A (2012) Septic shock attributed to Candida infection: importance of empiric therapy and source control. Clin Infect Dis 54(12):1739–1746
Garnacho-Montero J, Diaz-Martin A, Garcia-Cabrera E, de Ruiz Perez Pipaon M, Hernandez-Caballero C, Lepe-Jimenez JA (2013) Impact on hospital mortality of catheter removal and adequate antifungal therapy in Candida spp. bloodstream infections. J Antimicrob Chemother 68(1):206–213
Hsu DI, Nguyen M, Nguyen L, Law A, Wong-Beringer A (2010) A multicentre study to evaluate the impact of timing of caspofungin administration on outcomes of invasive candidiasis in non-immunocompromised adult patients. J Antimicrob Chemother 65(8):1765–1770
Kett DH, Shorr AF, Reboli AC, Reisman AL, Biswas P, Schlamm HT (2011) Anidulafungin compared with fluconazole in severely ill patients with candidemia and other forms of invasive candidiasis: support for the 2009 IDSA treatment guidelines for candidiasis. Crit Care 15(5):R253
Rex JH, Bennett JE, Sugar AM, Pappas PG, van der Horst CM, Edwards JE, Washburn RG, Scheld WM, Karchmer AW, Dine AP et al (1994) A randomized trial comparing fluconazole with amphotericin B for the treatment of candidemia in patients without neutropenia. Candidemia Study Group and the National Institute. N Engl J Med 331(20):1325–1330
Kuse ER, Chetchotisakd P, da Cunha CA, Ruhnke M, Barrios C, Raghunadharao D, Sekhon JS, Freire A, Ramasubramanian V, Demeyer I et al (2007) Micafungin versus liposomal amphotericin B for candidaemia and invasive candidosis: a phase III randomised double-blind trial. Lancet 369(9572):1519–1527
Alam FF, Mustafa AS, Khan ZU (2007) Comparative evaluation of (1, 3)-beta-d-glucan, mannan and anti-mannan antibodies, and Candida species-specific snPCR in patients with candidemia. BMC Infect Dis 7:103
Ostrosky-Zeichner L, Alexander BD, Kett DH, Vazquez J, Pappas PG, Saeki F, Ketchum PA, Wingard J, Schiff R, Tamura H et al (2005) Multicenter clinical evaluation of the (1–>3) beta-d-glucan assay as an aid to diagnosis of fungal infections in humans. Clin Infect Dis 41(5):654–659
Persat F, Ranque S, Derouin F, Michel-Nguyen A, Picot S, Sulahian A (2008) Contribution of the (1–>3)-beta-d-glucan assay for diagnosis of invasive fungal infections. J Clin Microbiol 46(3):1009–1013
Conflicts of interest
M.B. serves on scientific advisory boards for Pfizer Inc., Merck Serono, and Astellas Pharma Inc. and has received funding for travel or speaker honoraria from Pfizer Inc., Merck Serono, Gilead Sciences, Teva Inc., and Astellas Pharma Inc. C.T. has been paid for lectures and advisory boards for Pfizer, Novartis, Merck, Astellas, Gilead, Angelini, and Zambon Group. F.G.D.R., F.C., G.S., A.C., and M.T. have been speakers or consultants for Gilead Sciences, MSD, and Pfizer. T.J.W. has received research grants from Astellas, Novartis, Merck, ContraFect, and Pfizer and has been speaker or consultant for Astellas, ContraFect, Drais, iCo, Novartis, Pfizer, Methylgene, SigmaTau, and Trius. C.E. has served on advisory boards and received speaker honoraria from Pfizer Inc., Astellas Pharma Inc., and MSD. G.P. has received research grants from Gilead, Pfizer, Astellas, and MSD, has acted as paid consultant to Astellas, Gilead, and MSD, and is a member of the Astellas and MSD speaker’s bureaus. C.V. received grants as speaker/moderator in meetings sponsored by Pfizer, Gilead, MSD, Astellas, Abbott, Nadirex International, and BMS and received grants for participation in advisory boards by Gilead, Astellas, MSD, and Pfizer. Further, he obtained research grants for his institution from Pfizer, MSD, Gilead, Abbott, Jansen, BMS, and Novartis. D.H.K. serves as a consultant to and on scientific advisory boards for Pfizer Inc. and has received funding for travel or speaker honoraria from Pfizer Inc. The other authors serve on scientific advisory board of MSD. O.L. serves on scientific advisory boards for MSD and Astellas Pharma Inc. and has received speaker honoraria from Sanofi Aventis, Pfizer Inc., MSD, and Astellas Pharma Inc.
Author information
Authors and Affiliations
Corresponding author
Additional information
Take-home message: A group of clinical experts endorsed by the Italian Society of Intensive Care and the International Society of Chemotherapy elaborated specific statements and practice recommendations addressing the management of intra-abdominal invasive candidiasis based on the best direct and indirect evidence. International guidelines do not specifically address this particular clinical setting and scant direct evidence is available.
Rights and permissions
About this article
Cite this article
Bassetti, M., Marchetti, M., Chakrabarti, A. et al. A research agenda on the management of intra-abdominal candidiasis: results from a consensus of multinational experts. Intensive Care Med 39, 2092–2106 (2013). https://doi.org/10.1007/s00134-013-3109-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-013-3109-3