Abstract
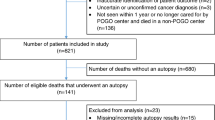
Autopsy findings of missed diagnoses that would probably have changed management or prognosis occur in up to 29% of cases in general hospitals. Such proportions may be higher in subsets of patients with complex diseases. We reviewed 2908 consecutive autopsies performed over a period of 29 months in a large-volume hospital, analyzing 118 autopsies of patients with hematological malignancies or severe aplastic anemia. A review of macroscopic reports as well as microscopic examination of tissue samples was performed. Medical records were reviewed for clinical diagnoses. Discordances between clinical and autopsy diagnoses were classified using Goldman’s criteria. Additionally, we searched for clinical parameters correlated with occurrence of class-I discrepancy using a multivariate method. Median age was 46.5 years, and 25.4% had received a hematopoietic stem-cell transplant. Overall, 11.9% (6.6–19.1%) of patients died before conclusion of the hematological diagnosis and 33% (24.6–42.3%) died with no active hematological disease. We found class-I discrepancy in 31.3% (23.1–40.5 %) of cases. The most common among these diagnoses were hematological disease, pneumonia and gastrointestinal bleeding. In a univariate analysis, being elderly (P=0.04) was positively correlated with the finding of class-I discrepancies; while, having received previous specific hematological treatment (P=0.0005) or hematopoietic stem-cell transplants (P=0.013), or being admitted to a specialized hematology unit (P=0.0006) were negatively correlated to the occurrence of such discrepancies. Multivariate analysis showed that care in a specialized hematology unit (OR 0.34, 0.12–0.93) was independently associated with lower occurrence of discrepancies. We concluded that critical diagnoses are often missed in highly complex hematological patients especially in the absence of admission to specialized hematology units.
Similar content being viewed by others
References
Ahronheim JC, Bernholc AS, Clark WD (1983) Age trends in autopsy rate. JAMA 250:1182–1186
Albanell J, Baselga J (2000) Systemic therapy emergencies. Semin Oncol 27:347–361
Anderson RE (1984) The autopsy as an instrument of quality assessment. Classification of premortem and postmortem diagnostic discrepancies. Arch Pathol Lab Med 108:490–493
Avgerinos DV, Bjornsson J (2001) Malignant neoplasms: discordance between clinical diagnoses and autopsy findings in 3,118 cases. APMIS 109:774–780
Battle RM, Pathak D, Humble MS, et al (1987) Factors influencing discrepancies between premortem and postmortem diagnoses. JAMA 258:339–344
Burton EC, Troxclair DA, Newman III WP (1998) Autopsy diagnoses of malignant neoplasms. How often are clinical diagnoses incorrect? JAMA 280:1245–1248
Campion EW, Reder VA, Mulley AG, Thibault GE (1986) Age and the declining rate of autopsy. J Am Geriatr Soc 34:865–868
Chandrasekar PH, Weinmann A, Shearer C (1995) Autopsy-identified infections among bone marrow transplant recipients: a clinico-pathologic study of 56 patients. Bone Marrow Transplant 16:675–681
Council on Scientific Affairs (1987) Autopsy — a comprehensive review of current issues. JAMA 258:364–369
Coradazzi AL, Morganti ALC, Montenegro MRG (2003) Discrepancies between clinical diagnosis and autopsy findings. Braz J Med Biol Res 36:385–391
Friederici HHR (1988) Reflections on the post mortem audit. JAMA 260:3461–3465
Friederici HHR, Sebastian M (1984) Autopsies in a modern teaching hospital. A review of 2,537 cases. Arch Pathol Lab Med 108:518–521
Gerain J, Sculier JP, Malengreaux A, Rykaert C, Themelin L (1990) Causes of deaths in an oncologic intensive care unit: a clinical and pathological study of 34 autopsies. Eur J Cancer 26:377–381
Goldman L, Sayson R, Robbins S, Cohn LH, Bettmann M, Weisberg M (1983) The value of the autopsy in three medical eras. N Engl J Med 308:1000–1005
Gough J (1985) Correlation between clinical and autopsy diagnosis in a community hospital. CMAJ 133:420–422
International Statistical Classification of Diseases and Related Health Problems, 1989 Revision, Geneva, World Health Organization, 1992
Kelly KM, Lange B (1997) Oncologic emergencies. Ped Oncol 44:809–830
Landefeld CS, Goldman L (1989) The autopsy in clinical medicine. Mayo Clin Proc 64:1185–1189
Landefeld CS, Chren MM, Myers A, Geller R, Robbins S, Goldman L (1988) Diagnostic yield of the autopsy in a university hospital and a community hospital. N Engl J Med 318:1249–1254
Marwick C (1995) Pathologists request autopsy revival. JAMA 273:1889–1891
McPhee SJ, Bottles K (1985) Autopsy: moribund art or vital science? Am J Med 78:107–113
Mort TC, Yeston NS (1999) The relationship of pre mortem diagnoses and post mortem findings in a surgical intensive care unit. Crit Care Med 27:299–303
Nemetz PN, Beard M, Ballard DJ, et al (1989) Resurrecting the autopsy: benefits and recommendations. Mayo Clin Proc 64:1065–1076
Nigro JF, Gresik MV, Fernbach J (1990) Value of the post mortem examination in a pediatric population with leukemia. J Pediatr 116:350–354
Nosari A, Barberis M, Landonio G, et al (1991) Infections in haematologic neoplasms: autopsy findings. Haematologica 76:135–140
de Pangher Manzini V, Revignas MG, Brollo A (1995) Diagnosis of malignant tumor: comparison between clinical and autopsy diagnoses. Hum Pathol 26:280–283
Provencio M, Espana P, Salas C, Navarro F, Bonilla F (2000) Hodgkin’s disease: correlation between causes of death at autopsy and clinical diagnosis. Ann Oncol 11:59–64
Pujol Farriols R, Bernet Vidal M, Castellsague J, Esquius Soriguera J, Raguer Sanz E, Yetano Laguna V (1994) Correlation between clinical and autopsy diagnosis at a general hospital. Ann Med Intern 11:372–376
Shojania KG, Burton EC, McDonald KM, Goldman L (2003) Changes in rates of autopsy-detected diagnostic errors over time. JAMA 298:2849–2856
Sun CC, Alonsonzana G, Love JC, Li L, Straumanis JP (2003) The value of autopsy in pediatric cardiology and cardiovascular surgery. Hum Pathol 34:491–496
Thurlbeck WM (1981) Accuracy of clinical diagnosis in a Canadian teaching hospital. CMAJ 125:443–447
Tse GM, Lee JC (2000) A 12 month review of autopsies performed at a university affiliated teaching hospital in Hong Kong. Hong Kong Med J 190–194
Veress B, Alafuzoff AI (1994) A retrospective analysis of clinical diagnoses and autopsy findings in 3,042 cases during two different time periods. Hum Pathol 25:140–145
Acknowledgements
We are in debt to Dr. Robert L. Gottlieb for careful review of this manuscript. ACGX received financial support from FAPESP (Fundação de Amparo à Pesquisa do Estado de São Paulo). L.J.M.C. received financial support from CAPES (Coordenação de Aperfeiçoamento de Pessoal de Nível Superior).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Xavier, A.C.G., Siqueira, S.A.C., Costa, L.J.M. et al. Missed diagnosis in hematological patients—an autopsy study. Virchows Arch 446, 225–231 (2005). https://doi.org/10.1007/s00428-004-1186-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-004-1186-y