Abstract
Background
Brunner’s gland proliferating lesions, termed Brunner’s gland hamartoma, hyperplasia, or adenoma, is regarded as a benign condition. However, cancerous changes have been reported in Brunner’s gland proliferating lesions.
Aims
The purpose of this study was to define the characteristic features of Brunner’s gland proliferating lesions and evaluate any observed cancerous changes.
Methods
We analysed clinicopathologic features and mucin expression in 25 Brunner’s gland proliferating lesions.
Results
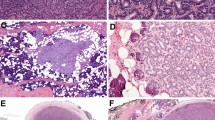
Brunner’s gland proliferating lesions were categorized as Brunner’s gland hamartoma or hyperplasia according to their tissue components. Brunner’s gland hamartoma commonly occurred in the duodenal bulb and exhibited a polypoid appearance, while Brunner’s gland hyperplasia was primarily observed in the second portion of duodenum as a submucosal mass and was accompanied by symptoms more frequently than Brunner’s gland hamartoma. The Brunner’s glands in Brunner’s gland proliferating lesions exhibited various morphologic characteristics, from normal-appearing glands to sclerotic glandular foci with atypia. Changes in MUC5 expression observed in both sclerotic glandular foci and dilated Brunner’s glands suggest that they might share a common mechanism and are associated with gastric foveolar metaplasia.
Conclusions
These findings indicate that most Brunner’s gland proliferating lesions are either hamartoma or hyperplasia, and that true neoplastic Brunner’s gland proliferating lesions are very rare. Thus, Brunner’s gland adenomas or carcinomas arising in Brunner’s gland proliferating lesions should be confirmed by ancillary tests, including immunostaining or molecular analysis, in addition to morphological criteria.



Similar content being viewed by others
References
Mills SE. Histology for Pathologists. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007.
Fenoglio-Preiser CM, Noffsinger AE, Stemmermann GN, Lantz PE, Isaacson PG. Gastrointestinal Pathology. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2008.
Botsford TW, Crowe P, Crocker DW. Tumors of the small intestine. A review of experience with 115 cases including a report of a rare case of malignant hemangio-endothelioma. Am J Surg. 1962;103:358–365.
Osborne R, Toffler R, Lowman RM. Brunner’s gland adenoma of the duodenum. Am J Dig Dis. 1973;18:689–694.
Levine JA, Burgart LJ, Batts KP, Wang KK. Brunner’s gland hamartomas: clinical presentation and pathological features of 27 cases. Am J Gastroenterol. 1995;90:290–294.
Chen YY, Su WW, Soon MS, Yen HH. Hemoclip-assisted polypectomy of large duodenal Brunner’s gland hamartoma. Dig Dis Sci. 2006;51:1670–1672.
Ohba R, Otaka M, Jin M, et al. Large Brunner’s gland hyperplasia treated with modified endoscopic submucosal dissection. Dig Dis Sci. 2007;52:170–172.
Akino K, Kondo Y, Ueno A, et al. Carcinoma of duodenum arising from Brunner’s gland. J Gastroenterol. 2002;37:293–296.
Itsuno M, Makiyama K, Omagari K, et al. Carcinoma of duodenal bulb arising from the Brunner’s gland. Gastroenterol Jpn. 1993;28:118–125.
Kushima R, Stolte M, Dirks K, et al. Gastric-type adenocarcinoma of the duodenal second portion histogenetically associated with hyperplasia and gastric-foveolar metaplasia of Brunner’s glands. Virchows Arch. 2002;440:655–659.
Shimizu N, Tanaka S, Morikawa J, et al. Early duodenal cancer of the bulb—report of a case. Gan No Rinsho. 1989;35:100–106.
Suzuki T, Ito A, Takayasu H, et al. A case of duodenal Brunner’s gland hyperplasia associated with in situ carcinoma. Nippon Shokakibyo Gakkai Zasshi. 1995;92:1189–1193.
Patel ND, Levy AD, Mehrotra AK, Sobin LH. Brunner’s gland hyperplasia and hamartoma: imaging features with clinicopathologic correlation. AJR Am J Roentgenol. 2006;187:715–722.
Giorgadze TA, Peterman H, Baloch ZW, et al. Diagnostic utility of mucin profile in fine-needle aspiration specimens of the pancreas: an immunohistochemical study with surgical pathology correlation. Cancer. 2006;108:186–197.
Ho SB, Shekels LL, Toribara NW, et al. Mucin gene expression in normal, preneoplastic, and neoplastic human gastric epithelium. Cancer Res. 1995;55:2681–2690.
Tamada S, Goto M, Nomoto M, et al. Expression of MUC1 and MUC2 mucins in extrahepatic bile duct carcinomas: its relationship with tumor progression and prognosis. Pathol Int. 2002;52:713–723.
Ando H, Aihara R, Ohno T, Ogata K, Mochiki E, Kuwano H. Prognostic significance of the expression of MUC1 and collagen type IV in advanced gastric carcinoma. Br J Surg. 2009;96:901–909.
Baldus SE, Monig SP, Huxel S, et al. MUC1 and nuclear beta-catenin are coexpressed at the invasion front of colorectal carcinomas and are both correlated with tumor prognosis. Clin Cancer Res. 2004;10:2790–2796.
Park SY, Roh SJ, Kim YN, et al. Expression of MUC1, MUC2, MUC5AC and MUC6 in cholangiocarcinoma: prognostic impact. Oncol Rep. 2009;22:649–657.
Brookes MJ, Manjunatha S, Allen CA, Cox M. Malignant potential in a Brunner’s gland hamartoma. Postgrad Med J. 2003;79:416–417.
Faller G, Kirchner T. Low-grade intraepithelial neoplasia of Brunner’s gland. Histopathology. 2005;47:118–119.
Fujimaki E, Nakamura S, Sugai T, Takeda Y. Brunner’s gland adenoma with a focus of p53-positive atypical glands. J Gastroenterol. 2000;35:155–158.
Sakurai T, Sakashita H, Honjo G, Kasyu I, Manabe T. Gastric foveolar metaplasia with dysplastic changes in Brunner gland hyperplasia: possible precursor lesions for Brunner gland adenocarcinoma. Am J Surg Pathol. 2005;29:1442–1448.
Zanetti G, Casadei G. Brunner’s gland hamartoma with incipient ductal malignancy. Report of a case. Tumori. 1981;67:75–78.
Fisher JK. Mucocele of a Brunner gland. Radiology. 1980;136:320.
Golan J, Dollberg L, Dollberg M, Farkash T, Rivkin L. Cystic hamartoma of Brunner’s glands. Int Surg. 1978;63:173–175.
Powers M, Sayuk GS, Wang HL. Brunner gland cyst: report of three cases. Int J Clin Exp Pathol. 2008;1:536–538.
Taura M, Taura S, Kummerow FA, Noritomi S, Iwanaga S. An ultrastructural study of the Brunner’s cyst. Gastroenterol Jpn. 1977;12:241–244.
Wolk DP, Knapper WH, Farr GH. Brunner’s gland cystadenoma of the duodenum. Am J Surg. 1973;126:439–440.
Chang MS, Kim WH, Kim YI. Brunner’s gland hamartoma. A clinicopathologic analysis of six cases. Korean J Gastrointest Endosc. 1994;14:19–23.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, K., Jang, S.J., Song, H.J. et al. Clinicopathologic Characteristics and Mucin Expression in Brunner’s Gland Proliferating Lesions. Dig Dis Sci 58, 194–201 (2013). https://doi.org/10.1007/s10620-012-2320-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-012-2320-3