Key Points
-
Urothelial tumours arise and evolve through divergent phenotypic pathways. Some tumours progress from urothelial hyperplasia to low-grade non-invasive superficial papillary tumours. More aggressive variants arise either from flat, high-grade carcinoma in situ and progress to invasive tumours, or they arise de novo as invasive tumours.
-
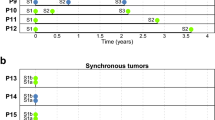
These two important phenotypic variants of urothelial tumours exhibit drastically different biological behaviours and prognoses. The low-grade papillary variant is often multifocal and tends to recur, but it infrequently progresses to muscle invasive stages, whereas most of the invasive variants develop into incurable metastases despite radical cystectomy.
-
It is becoming clear that the two urothelial tumour variants harbour distinctive genetic defects: the low-grade non-invasive papillary tumours are characterized by activating mutations in the HRAS gene and fibroblast growth factor receptor 3 gene; and the high-grade invasive tumours are characterized by structural and functional defects in the p53 and retinoblastoma protein (RB) tumour-suppressor pathways.
-
The deletion of both arms of chromosome 9 is prevalent in urothelial carcinomas and occurs during the earliest stages of tumorigenesis. However, these chromosomal aberrations do not seem to distinguish between the two tumour development pathways.
-
Tumour invasion and progression in the bladder seems to be a multifactorial process, promoted by microenvironmental changes that include the upregulation of N-cadherin, the downregulation of E-cadherin, the overexpression of matrix metalloproteinases 2 and 9, an imbalance between angiogenic and anti-angiogenic factors, and increased synthesis of prostaglandin.
-
Urothelial carcinomas are particularly amenable to pathway- and target-based therapies. The low-grade non-invasive papillary tumours could benefit tremendously from receptor tyrosine kinase (RTK)–Ras pathway inhibition by means such as small molecule inhibitors, monoclonal antibodies, farnesyl and geranylgeranyl inhibitors, and RAF and mitogen-activated protein kinase kinase (MEK) inhibitors. The invasive tumours, on the other hand, could benefit from replacement therapies that restore the functions of p53 and RB.
-
The intravesical (within the bladder) route of drug delivery provides a unique advantage because it locally enriches the drug while preventing systemic toxicity in urothelial carcinoma treatment.
-
The identification of specific carcinogens that precipitate each urothelial tumour pathway holds the key to eventually preventing this disease from occurring.
Abstract
Urothelial carcinoma of the bladder is unique among epithelial carcinomas in its divergent pathways of tumorigenesis. Low-grade papillary tumours rarely become muscle-invasive and they frequently harbour gene mutations that constitutively activate the receptor tyrosine kinase–Ras pathway. By contrast, most high-grade invasive tumours progress to life-threatening metastases and have defects in the p53 and the retinoblastoma protein pathways. Correcting pathway-specific defects represents an attractive strategy for the molecular therapy of urothelial carcinomas.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Parkin, D. M., Bray, F., Ferlay, J. & Pisani, P. Estimating the world cancer burden: Globocan 2000. Int. J. Cancer 94, 153–156 (2001).
Johansson, S. L. & Cohen, S. M. Epidemiology and etiology of bladder cancer. Semin. Surg. Oncol. 13, 291–298 (1997). Comprehensive review of risk factors and potential chemical carcinogens associated with the development of urothelial carcinomas.
Hanahan, D. & Weinberg, R. A. The hallmarks of cancer. Cell 100, 57–70 (2000).
Kinzler, K. W. & Vogelstein, B. Lessons from hereditary colorectal cancer. Cell 87, 159–170 (1996).
Koss, L. G. Bladder cancer from a perspective of 40 years. J. Cell. Biochem. Suppl. 16I, 23–29 (1992). One of the pioneering reports using classical clinicopathological observations to indicate that the urothelium develops tumours along two distinctive pathways.
Sauter, G. et al. in World Health Organization Classification of Tumors. Pathology and Genetics: Tumors of the Urinary System and Male Genital Organs. (eds Eble, J. N., Sauter, G., Epstein, J. I. & Sesterhenn, I.) PP110 (IARCC Press, Lyon, 2004).
Steinberg, G. D., Trump, D. L. & Cummings, K. B. Metastatic bladder cancer. Natural history, clinical course, and consideration for treatment. Urol. Clin. North Am. 19, 735–746 (1992).
Liebert, M. & Seigne, J. Characteristics of invasive bladder cancers: histological and molecular markers. Semin. Urol. Oncol. 14, 62–72 (1996).
Dalbagni, G., Presti, J., Reuter, V., Fair, W. R. & Cordon-Cardo, C. Genetic alterations in bladder cancer. Lancet 342, 469–471 (1993).
Egger, G., Liang, G., Aparicio, A. & Jones, P. A. Epigenetics in human disease and prospects for epigenetic therapy. Nature 429, 457–463 (2004). Overview of the mechanisms of epigenetic gene silencing, such as DNA methylation and deacetylation. This paper discusses epigenetic diseases and emerging therapies based on the inhibition of DNA methyltransferases and histone deacetylases.
Dinney, C. P. et al. Focus on bladder cancer. Cancer Cell 6, 111–116. (2004). Comprehensive review of urothelial carcinomas focusing on disease pathogenesis, experimental models, diagnosis and clinical therapies.
Gschwind, A., Fischer, O. M. & Ullrich, A. The discovery of receptor tyrosine kinases: targets for cancer therapy. Nature Rev. Cancer 4, 361–370 (2004). In-depth review of RTK family proteins, including their structure, function, signalling pathways, their roles in tumorigenesis and their anti-RTK strategies in cancer treatment.
Reddy, E. P., Reynolds, R. K., Santos, E. & Barbacid, M. A point mutation is responsible for the acquisition of transforming properties by the T24 human bladder carcinoma oncogene. Nature 300, 149–152 (1982).
Czerniak, B. et al. Concurrent mutations of coding and regulatory sequences of the Ha-ras gene in urinary bladder carcinomas. Hum. Pathol. 23, 1199–1204 (1992).
Knowles, M. A. & Williamson, M. Mutation of H-ras is infrequent in bladder cancer: confirmation by single-strand conformation polymorphism analysis, designed restriction fragment length polymorphisms, and direct sequencing. Cancer Res. 53, 133–139 (1993).
Fitzgerald, J. M. et al. Identification of H-ras mutations in urine sediments complements cytology in the detection of bladder tumors. J. Natl Cancer Inst. 87, 129–133 (1995).
Feinberg, A. P., Vogelstein, B., Droller, M. J., Baylin, S. B. & Nelkin, B. D. Mutation affecting the 12th amino acid of the c-Ha-ras oncogene product occurs infrequently in human cancer. Science 220, 1175–1177 (1983).
Przybojewska, B., Jagiello, A. & Jalmuzna, P. H-RAS, K-RAS, and N-RAS gene activation in human bladder cancers. Cancer Genet. Cytogenet. 121, 73–77 (2000).
Zhu, D., Xing, D., Shen, X. & Liu, J. A method to quantitatively detect H-ras point mutation based on electrochemiluminescence. Biochem. Biophys. Res. Commun. 324, 964–969 (2004).
Buyru, N., Tigli, H., Ozcan, F. & Dalay, N. Ras oncogene mutations in urine sediments of patients with bladder cancer. J. Biochem. Mol. Biol. 36, 399–402 (2003).
Lin, J. H., Zhao, H. & Sun, T. T. A tissue-specific promoter that can drive a foreign gene to express in the suprabasal urothelial cells of transgenic mice. Proc. Natl Acad. Sci. USA 92, 679–683 (1995).
Zhang, Z. T. et al. Role of Ha-ras activation in superficial papillary pathway of urothelial tumor formation. Oncogene 20, 1973–1980 (2001).
Ye, D. W., Zheng, J. F., Qian, S. X. & Ma, Y. J. Correlation between the expression of oncogenes ras and c-erbB-2 and the biological behavior of bladder tumors. Urol. Res. 21, 39–43 (1993).
Cappellen, D. et al. Frequent activating mutations of FGFR3 in human bladder and cervix carcinomas. Nature Genet. 23, 18–20 (1999). First report demonstrating FGFR3 mutations (which were previously associated with skeletal developmental disorders) in solid tumours, including urothelial and cervical carcinomas. Screening of all coding regions showed mutations concentrated in exons 7, 10 and 15.
Ornitz, D. M. & Itoh, N. Fibroblast growth factors. Genome Biol. 2, REVIEWS 3005.1–3005.12 (2001).
Wilkie, A. O., Patey, S. J., Kan, S. H., van den Ouweland, A. M. & Hamel, B. C. FGFs, their receptors, and human limb malformations: clinical and molecular correlations. Am. J. Med. Genet. 112, 266–278 (2002).
Sibley, K., Stern, P. & Knowles, M. A. Frequency of fibroblast growth factor receptor 3 mutations in sporadic tumours. Oncogene 20, 4416–4418 (2001).
Fracchiolla, N. S. et al. FGFR3 gene mutations associated with human skeletal disorders occur rarely in multiple myeloma. Blood 92, 2987–2989 (1998).
Wu, R. et al. Somatic mutations of fibroblast growth factor receptor 3 (FGFR3) are uncommon in carcinomas of the uterine cervix. Oncogene 19, 5543–5546 (2000).
Rieger-Christ, K. M. et al. Identification of fibroblast growth factor receptor 3 mutations in urine sediment DNA samples complements cytology in bladder tumor detection. Cancer 98, 737–744 (2003).
van Rhijn, B. W. et al. FGFR3 and p53 characterize alternative genetic pathways in the pathogenesis of urothelial cell carcinoma. Cancer Res, 64, 1911–1914 (2004).
Bakkar, A. A. et al. FGFR3 and TP53 gene mutations define two distinct pathways in urothelial cell carcinoma of the bladder. Cancer Res. 63, 8108–8112 (2003).
van Rhijn, B. W., Montironi, R., Zwarthoff, E. C., Jobsis, A. C. & van der Kwast, T. H. Frequent FGFR3 mutations in urothelial papilloma. J. Pathol. 198, 245–251 (2002).
Billerey, C. et al. Frequent FGFR3 mutations in papillary non-invasive bladder (pTa) tumors. Am. J. Pathol. 158, 1955–1959 (2001).
Cho, J. Y. et al. Defective lysosomal targeting of activated fibroblast growth factor receptor 3 in achondroplasia. Proc. Natl Acad. Sci. USA 101, 609–614 (2004).
Monsonego-Ornan, E., Adar, R., Feferman, T., Segev, O. & Yayon, A. The transmembrane mutation G380R in fibroblast growth factor receptor 3 uncouples ligand-mediated receptor activation from down-regulation. Mol. Cell Biol. 20, 516–522 (2000).
Agazie, Y. M., Movilla, N., Ischenko, I. & Hayman, M. J. The phosphotyrosine phosphatase SHP2 is a critical mediator of transformation induced by the oncogenic fibroblast growth factor receptor 3. Oncogene 22, 6909–6918 (2003).
Kanai, M., Goke, M., Tsunekawa, S. & Podolsky, D. K. Signal transduction pathway of human fibroblast growth factor receptor 3. Identification of a novel 66-kDa phosphoprotein. J. Biol. Chem. 272, 6621–6628 (1997).
Yasoda, A. et al. Overexpression of CNP in chondrocytes rescues achondroplasia through a MAPK-dependent pathway. Nature Med. 10, 80–86 (2004).
Hart, K. C., Robertson, S. C. & Donoghue, D. J. Identification of tyrosine residues in constitutively activated fibroblast growth factor receptor 3 involved in mitogenesis, Stat activation, and phosphatidylinositol 3-kinase activation. Mol. Biol. Cell 12, 931–942 (2001).
Hart, K. C. et al. Transformation and Stat activation by derivatives of FGFR1, FGFR3, and FGFR4. Oncogene 19, 3309–3320 (2000).
Memon, A. A. et al. Expression of HER3, HER4 and their ligand heregulin-4 is associated with better survival in bladder cancer patients. Br. J. Cancer 91, 2034–2041 (2004).
Lipponen, P. & Eskelinen, M. Expression of epidermal growth factor receptor in bladder cancer as related to established prognostic factors, oncoprotein (c-erbB-2, p53) expression and long-term prognosis. Br. J. Cancer 69, 1120–1125 (1994).
Messing, E. M. Growth factors and bladder cancer: clinical implications of the interactions between growth factors and their urothelial receptors. Semin. Surg. Oncol. 8, 285–292 (1992).
Coogan, C. L., Estrada, C. R., Kapur, S. & Bloom, K. J. HER-2/neu protein overexpression and gene amplification in human transitional cell carcinoma of the bladder. Urology 63, 786–790 (2004).
Sandberg, A. A. Cytogenetics and molecular genetics of bladder cancer: a personal view. Am. J. Med. Genet. 115, 173–182 (2002).
Stoehr, R. et al. Deletions of chromosomes 9 and 8p in histologically normal urothelium of patients with bladder cancer. Eur. Urol. 47, 58–63 (2005).
Spruck, C. H. R. et al. Two molecular pathways to transitional cell carcinoma of the bladder. Cancer Res. 54, 784–788 (1994).
Obermann, E. C. et al. Frequent genetic alterations in flat urothelial hyperplasias and concomitant papillary bladder cancer as detected by CGH, LOH, and FISH analyses. J. Pathol. 199, 50–57 (2003).
Chow, N. H. et al. Papillary urothelial hyperplasia is a clonal precursor to papillary transitional cell bladder cancer. Int. J. Cancer 89, 514–518 (2000).
Hartmann, A. et al. Frequent genetic alterations in simple urothelial hyperplasias of the bladder in patients with papillary urothelial carcinoma. Am. J. Pathol. 154, 721–727 (1999).
Hartmann, A. et al. Occurrence of chromosome 9 and p53 alterations in multifocal dysplasia and carcinoma in situ of human urinary bladder. Cancer Res. 62, 809–818 (2002).
Sherr, C. J. The INK4a/ARF network in tumour suppression. Nature Rev. Mol. Cell Biol. 2, 731–737 (2001).
Baud, E., Catilina, P. & Bignon, Y. J. p16 involvement in primary bladder tumors: analysis of deletions and mutations. Int. J. Oncol. 14, 441–445 (1999).
Orlow, I. et al. Deletion of the p16 and p15 genes in human bladder tumors. J. Natl Cancer Inst. 87, 1524–1529 (1995).
Gonzalez-Zulueta, M. et al. Methylation of the 5′CpG island of the p16/CDKN2 tumor suppressor gene in normal and transformed human tissues correlates with gene silencing. Cancer Res. 55, 4531–4535 (1995).
Gonzalgo, M. L. et al. The role of DNA methylation in expression of the p19/p16 locus in human bladder cancer cell lines. Cancer Res. 58, 1245–1252 (1998).
Serrano, M. et al. Role of the INK4a locus in tumor suppression and cell mortality. Cell 85, 27–37 (1996).
Kamijo, T. et al. Tumor suppression at the mouse INK4a locus mediated by the alternative reading frame product p19ARF. Cell 91, 649–659 (1997).
Sharpless, N. E. et al. Loss of p16Ink4a with retention of p19Arf predisposes mice to tumorigenesis. Nature 413, 86–91 (2001).
Knowles, M. A., Habuchi, T., Kennedy, W. & Cuthbert-Heavens, D. Mutation spectrum of the 9q34 tuberous sclerosis gene TSC1 in transitional cell carcinoma of the bladder. Cancer Res. 63, 7652–7656 (2003).
Knowles, M. A., Shaw, M. E. & Proctor, A. J. Deletion mapping of chromosome 8 in cancers of the urinary bladder using restriction fragment length polymorphisms and microsatellite polymorphisms. Oncogene 8, 1357–1364 (1993).
Natrajan, R., Louhelainen, J., Williams, S., Laye, J. & Knowles, M. A. High-resolution deletion mapping of 15q13. 2-q21. 1 in transitional cell carcinoma of the bladder. Cancer Res. 63, 7657–7662 (2003).
Cordon-Cardo, C. Molecular alterations in bladder cancer. Cancer Surv. 32, 115–131 (1998).
Lu, M. L. et al. Impact of alterations affecting the p53 pathway in bladder cancer on clinical outcome, assessed by conventional and array-based methods. Clin. Cancer Res. 8, 171–179 (2002).
Stein, J. P. et al. Effect of p21WAF1/CIP1 expression on tumor progression in bladder cancer. J. Natl Cancer Inst. 90, 1072–1079 (1998).
Feng, Z., Hu, W., Rom, W. N., Beland, F. A. & Tang, M. S. 4-aminobiphenyl is a major etiological agent of human bladder cancer: evidence from its DNA binding spectrum in human p53 gene. Carcinogenesis 23, 1721–1727 (2002).
Orntoft, T. F. & Wolf, H. Molecular alterations in bladder cancer. Urol. Res. 26, 223–233 (1998).
Cordon-Cardo, C. et al. p53 mutations in human bladder cancer: genotypic versus phenotypic patterns. Int. J. Cancer 56, 347–353 (1994).
Hruban, R. H., van der Riet, P., Erozan, Y. S. & Sidransky, D. Brief report: molecular biology and the early detection of carcinoma of the bladder--the case of Hubert H. Humphrey. N. Engl. J. Med. 330, 1276–1278 (1994).
Wagner, U. et al. Patterns of p53, erbB-2, and EGF-r expression in premalignant lesions of the urinary bladder. Hum. Pathol. 26, 970–978 (1995).
Esrig, D. et al. Accumulation of nuclear p53 and tumor progression in bladder cancer. N. Engl. J. Med. 331, 1259–1264 (1994).
Cordon-Cardo, C. Cell cycle regulators as prognostic factors for bladder cancer. Eur. Urol. 33, 11–12 (1998).
Masters, J. R. et al. Can p53 staining be used to identify patients with aggressive superficial bladder cancer? J. Pathol. 200, 74–81 (2003).
Shariat, S. F. et al. p53, p21, pRb, and p16 expression predict clinical outcome in cystectomy with bladder cancer. J. Clin. Oncol. 22, 1014–1024 (2004).
Hinata, N. et al. Radiation induces p53-dependent cell apoptosis in bladder cancer cells with wild-type- p53 but not in p53-mutated bladder cancer cells. Urol. Res. 31, 387–396 (2003).
Shiraishi, K., Eguchi, S., Mohri, J. & Kamiryo, Y. P53 mutation predicts intravesical adriamycin instillation failure in superficial transitional cell carcinoma of bladder. Anticancer Res. 23, 3475–3478 (2003).
Cote, R. J., Esrig, D., Groshen, S., Jones, P. A. & Skinner, D. G. p53 and treatment of bladder cancer. Nature 385, 123–125 (1997). In a trial of adjuvant chemotherapy for patients with invasive urothelial carcinomas, only those that exhibited altered p53 expression responded to therapy. This landmark study forms the basis for an ongoing multicentre clinical trial on p53-targeted therapy trial in bladder cancer.
Donehower, L. A. et al. Mice deficient for p53 are developmentally normal but susceptible to spontaneous tumours. Nature 356, 215–221 (1992).
Gao, J. et al. p53 deficiency provokes urothelial proliferation and synergizes with activated HA-RAS in promoting urothelial tumorigenesis. Oncogene 23, 687–696 (2004).
Piette, J., Neel, H. & Marechal, V. Mdm2: keeping p53 under control. Oncogene 15, 1001–1010 (1997).
Korkolopoulou, P. et al. The role of p53, MDM2 and c-erb B-2 oncoproteins, epidermal growth factor receptor and proliferation markers in the prognosis of urinary bladder cancer. Pathol. Res. Pract. 193, 767–775 (1997).
Simon, R. et al. Amplification pattern of 12q13–q15 genes (MDM2, CDK4, GLI) in urinary bladder cancer. Oncogene 21, 2476–2483 (2002).
Fletcher, O. et al. Lifetime risks of common cancers among retinoblastoma survivors. J. Natl Cancer Inst. 96, 357–363 (2004).
Cairns, P., Proctor, A. J. & Knowles, M. A. Loss of heterozygosity at the RB locus is frequent and correlates with muscle invasion in bladder carcinoma. Oncogene 6, 2305–2309 (1991).
Chatterjee, S. J. et al. Hyperphosphorylation of pRb: a mechanism for RB tumour suppressor pathway inactivation in bladder cancer. J. Pathol. 203, 762–770 (2004).
Logothetis, C. J. et al. Altered expression of retinoblastoma protein and known prognostic variables in locally advanced bladder cancer. J. Natl Cancer Inst. 84, 1256–12561 (1992).
Hernando, E. et al. Rb inactivation promotes genomic instability by uncoupling cell cycle progression from mitotic control. Nature 430, 797–802 (2004). Provides direct evidence that MAD2 is a major target of E2F and that RB inactivation leads to increased activity of E2F, and then MAD2 overexpression and aneuploidy.
Cote, R. J. et al. Elevated and absent pRb expression is associated with bladder cancer progression and has cooperative effects with p53. Cancer Res. 58, 1090–1094 (1998).
Grossman, H. B. et al. p53 and Rb expression predict progression in T1 bladder cancer. Clin. Cancer Res. 4, 829–834 (1998).
Cordon-Cardo, C. et al. Cooperative effects of p53 and pRB alterations in primary superficial bladder tumors. Cancer Res. 57, 1217–1221 (1997).
Chatterjee, S. J. et al. Combined effects of p53, p21, and pRb expression in the progression of bladder transitional cell carcinoma. J. Clin. Oncol. 22, 1007–1013 (2004).
Pipas, J. M. & Levine, A. J. Role of T antigen interactions with p53 in tumorigenesis. Semin. Cancer Biol. 11, 23–30 (2001).
Zhang, Z. T., Pak, J., Shapiro, E., Sun, T. T. & Wu, X. R. Urothelium-specific expression of an oncogene in transgenic mice induced the formation of carcinoma in situ and invasive transitional cell carcinoma. Cancer Res. 59, 3512–3517 (1999).
Grippo, P. J. & Sandgren, E. P. Highly invasive transitional cell carcinoma of the bladder in a simian virus 40 T-antigen transgenic mouse model. Am. J. Pathol. 157, 805–813 (2000).
Garcia del Muro, X. et al. Prognostic value of the expression of E-cadherin and β-catenin in bladder cancer. Eur. J. Cancer 36, 357–362 (2000).
Shariat, S. F. et al. E-cadherin expression predicts clinical outcome in carcinoma in situ of the urinary bladder. Urology 57, 60–65 (2001).
Popov, Z. et al. Low E-cadherin expression in bladder cancer at the transcriptional and protein level provides prognostic information. Br. J. Cancer 83, 209–214 (2000).
Ribeiro-Filho, L. A., et al. CpG hypermethylation of promoter region and inactivation of E-cadherin gene in human bladder cancer. Mol. Carcinog. 34, 187–198 (2002).
Zhang, X. et al. Association between a C/A single nucleotide polymorphism of the E-cadherin gene promoter and transitional cell carcinoma of the bladder. J. Urol. 170, 1379–1382 (2003).
Sanchez-Carbayo, M. et al. Molecular profiling of bladder cancer using cDNA microarrays: defining histogenesis and biological phenotypes. Cancer Res. 62, 6973–6980 (2002).
Rieger-Christ, K. M. et al. Novel expression of N-cadherin elicits in vitro bladder cell invasion via the Akt signaling pathway. Oncogene 23, 4745–4753 (2004).
Vihinen, P. & Kahari, V. M. Matrix metalloproteinases in cancer: prognostic markers and therapeutic targets. Int. J. Cancer 99, 157–166 (2002).
Kanayama, H. Matrix metalloproteinases and bladder cancer. J. Med. Invest. 48, 31–43 (2001).
Izawa, J. I. et al. Differential expression of progression-related genes in the evolution of superficial to invasive transitional cell carcinoma of the bladder. Oncol. Rep. 8, 9–15 (2001).
Slaton, J. W. et al. Treatment with low-dose interferon-a restores the balance between matrix metalloproteinase-9 and E-cadherin expression in human transitional cell carcinoma of the bladder. Clin. Cancer Res. 7, 2840–2853 (2001).
Campbell, S. C., Volpert, O. V., Ivanovich, M. & Bouck, N. P. Molecular mediators of angiogenesis in bladder cancer. Cancer Res. 58, 1298–3104 (1998).
Grossfeld, G. D. et al. Thrombospondin-1 expression in bladder cancer: association with p53 alterations, tumor angiogenesis, and tumor progression. J. Natl Cancer Inst. 89, 219–227 (1997).
Komhoff, M. et al. Enhanced expression of cyclooxygenase-2 in high grade human transitional cell bladder carcinomas. Am. J. Pathol. 157, 29–35 (2000).
Sebolt-Leopold, J. S. & Herrera, R. Targeting the mitogen-activated protein kinase cascade to treat cancer. Nature Rev. Cancer 4, 937–947 (2004). In-depth review of how MAPK pathway components are being exploited for target-based therapies. Summarizes the mechanisms, therapeutic effects and challenges of the use of inhibitors against farnesyltransferases, RAF and MEK.
Downward, J. Targeting RAS signalling pathways in cancer therapy. Nature. Rev. Cancer 3, 11–22 (2003). Reviews upstream and downstream signals of RAS, the role of Ras pathway activation in tumorigenesis, and therapeutic strategies targeting various components of the Ras pathway.
Bellmunt, J., Hussain, M. & Dinney, C. P. Novel approaches with targeted therapies in bladder cancer. Therapy of bladder cancer by blockade of the epidermal growth factor receptor family. Crit. Rev. Oncol. Hematol. 46 (Suppl.), S85–S104 (2003).
Laird, A. D. et al. SU6668 is a potent antiangiogenic and antitumor agent that induces regression of established tumors. Cancer Res. 60, 4152–4160 (2000).
Mohammadi, M. et al. Structures of the tyrosine kinase domain of fibroblast growth factor receptor in complex with inhibitors. Science 276, 955–960 (1997). By screening a library of synthetic compounds, the authors identified a new class of inhibitors (belonging to indolinones) for RTKs. Crystal structures showed that the compounds occupy the ATP binding site of the tyrosine kinase domain of FGFR1.
Paterson, J. L. et al. Preclinical studies of fibroblast growth factor receptor 3 as a therapeutic target in multiple myeloma. Br. J. Haematol. 124, 595–603 (2004).
Grand, E. K., Chase, A. J., Heath, C., Rahemtulla, A. & Cross, N. C. Targeting FGFR3 in multiple myeloma: inhibition of t(4;14)-positive cells by SU5402 and PD173074. Leukemia 18, 962–966 (2004).
Mohammadi, M. et al. Crystal structure of an angiogenesis inhibitor bound to the FGF receptor tyrosine kinase domain. EMBO J. 17, 5896–5904 (1998).
Trudel, S. et al. Inhibition of fibroblast growth factor receptor 3 induces differentiation and apoptosis in t(4;14) myeloma. Blood 103, 3521–3528 (2004).
Trudel, S. et al. CHIR-258, a novel, multi-targeted tyrosine kinase inhibitor for the potential treatment of t(4;14) multiple myeloma. Blood 105, 2941–2948 (2005).
Gomez-Roman, J. J. et al. Fibroblast growth factor receptor 3 Is overexpressed in urinary tract carcinomas and modulates the neoplastic cell growth. Clin. Cancer Res. 11, 459–465 (2005).
Rauchenberger, R. et al. Human combinatorial Fab library yielding specific and functional antibodies against the human fibroblast growth factor receptor 3. J. Biol. Chem. 278, 38194–38205 (2003).
Sebti, S. M. & Adjei, A. A. Farnesyltransferase inhibitors. Semin. Oncol. 31, 28–39 (2004).
Brunner, T. B. et al. Farnesyltransferase inhibitors: an overview of the results of preclinical and clinical investigations. Cancer Res. 63, 5656–5668 (2003). Discusses the mechanisms and potential targets of farnesyltransferase inhibitors and summarizes completed and ongoing clinical trials using these inhibitors.
Lobell, R. B. et al. Evaluation of farnesyl:protein transferase and geranylgeranyl:protein transferase inhibitor combinations in preclinical models. Cancer Res. 61, 8758–8768 (2001).
Cohen-Jonathan, E. et al. Farnesyltransferase inhibitors potentiate the antitumor effect of radiation on a human tumor xenograft expressing activated HRAS. Radiat. Res. 154, 125–132 (2000).
Allen, L. F., Sebolt-Leopold, J. & Meyer, M. B. CI-1040 (PD184352), a targeted signal transduction inhibitor of MEK (MAPKK). Semin. Oncol. 30, 105–116 (2003).
Hsieh, J. T., Dinney, C. P. & Chung, L. W. The potential role of gene therapy in the treatment of bladder cancer. Urol. Clin. North Am. 27, 103–113 (2000).
Pagliaro, L. C. Gene therapy for bladder cancer. World J. Urol. 18, 148–151 (2000).
Kuball, J. et al. Successful adenovirus-mediated wild-type p53 gene transfer in patients with bladder cancer by intravesical vector instillation. J. Clin. Oncol. 20, 957–965 (2002).
Pagliaro, L. C. et al. Repeated intravesical instillations of an adenoviral vector in patients with locally advanced bladder cancer: a phase I study of p53 gene therapy. J. Clin. Oncol. 21, 2247–2253 (2003).
Siemens, D. R., Crist, S., Austin, J. C., Tartaglia, J. & Ratliff, T. L. Comparison of viral vectors: gene transfer efficiency and tissue specificity in a bladder cancer model. J. Urol. 170, 979–984 (2003).
Li, Y. et al. Loss of adenoviral receptor expression in human bladder cancer cells: a potential impact on the efficacy of gene therapy. Cancer Res. 59, 325–330 (1999).
Fodor, I. et al. Vaccinia virus mediated p53 gene therapy for bladder cancer in an orthotopic murine model. J. Urol. 173, 604–609 (2005).
Kikuchi, E. et al. Inhibition of orthotopic human bladder tumor growth by lentiviral gene transfer of endostatin. Clin. Cancer Res. 10, 1835–1842 (2004).
McNeish, I. A., Bell, S. J. & Lemoine, N. R. Gene therapy progress and prospects: cancer gene therapy using tumour suppressor genes. Gene Therapy 11, 497–503 (2004).
Foster, B. A., Coffey, H. A., Morin, M. J. & Rastinejad, F. Pharmacological rescue of mutant p53 conformation and function. Science 286, 2507–2510 (1999). The mass screening of a library of synthetic compounds identified a prototypic chemical labelled CP-31398, which was capable of stabilizing wild-type p53 and nascent (but not preformed) p53 mutant, and of inhibiting tumour growth in vitro and in vivo.
Bykov, V. J. et al. Restoration of the tumor suppressor function to mutant p53 by a low-molecular-weight compound. Nature Med. 8, 282–288 (2002). A compound termed PRIMA 1 was discovered through screening of a chemical library based on growth suppression of tumour cells. PRIMA 1 was capable of restoring the conformational structure, DNA binding activity and target-gene transcription of mutant p53, and inhibiting tumour growth in vivo.
Demma, M. J., Wong, S., Maxwell, E. & Dasmahapatra, B. CP-31398 restores DNA-binding activity to mutant p53 in vitro but does not affect p53 homologs p63 and p73. J. Biol. Chem. 279, 45887–45896 (2004).
Luu, Y., Bush, J., Cheung, K. J. Jr & Li, G. The p53 stabilizing compound CP-31398 induces apoptosis by activating the intrinsic Bax/mitochondrial/caspase-9 pathway. Exp. Cell Res. 276, 214–222 (2002).
Cordon-Cardo, C. & Reuter, V. E. Alterations of tumor suppressor genes in bladder cancer. Semin. Diagn. Pathol. 14, 123–132 (1997).
Zhang, X. et al. Adenoviral-mediated retinoblastoma 94 produces rapid telomere erosion, chromosomal crisis, and caspase-dependent apoptosis in bladder cancer and immortalized human urothelial cells but not in normal urothelial cells. Cancer Res. 63, 760–765 (2003).
Li, D. et al. The role of adenovirus-mediated retinoblastoma 94 in the treatment of head and neck cancer. Cancer Res. 62, 4637–4644 (2002).
Cordon-Cardo, C., Cote, R. J. & Sauter, G. Genetic and molecular markers of urothelial premalignancy and malignancy. Scand. J. Urol. Nephrol. (Suppl.) 205, 82–93 (2000).
Jonkers, J. & Berns, A. Conditional mouse models of sporadic cancer. Nature Rev. Cancer 2, 251–265 (2002).
Wallerand, H. et al. Mutations in TP53, but not FGFR3, in urothelial cell carcinoma of the bladder are influenced by smoking: contribution of exogenous versus endogenous carcinogens. Carcinogenesis 26, 177–184 (2005).
Acknowledgements
The author wishes to acknowledge the useful discussion/comments by members of his laboratory and his collaborators. Research in the author's laboratory is supported by grants from the United States National Institutes of Health and Veterans' Administration. The author regrets that due to space limitation many important studies could not be cited in the article.
Author information
Authors and Affiliations
Ethics declarations
Competing interests
The author declares no competing financial interests.
Related links
Related links
DATABASES
Entrez Gene
National Cancer Institute
FURTHER INFORMATION
American Urological Association homepage
National Cancer Institute progress report on kidney and bladder cancers
Glossary
- HYPERPLASIA
-
An increase in the number of cells in a tissue or organ without corresponding gross morphological changes.
- ANEUSOMY
-
Having an abnormal number of chromosomes. Most human epithelial cancers harbour genomes that are characterized by gross aneusomy.
- LOSS OF HETEROZYGOSITY
-
In cells that carry a mutated allele of a tumour-suppressor gene, the gene becomes fully inactivated when the cell loses a large part of the chromosome carrying the wild-type allele. Regions with high frequency of loss of heterozygosity are believed to harbour tumour-suppressor genes.
- COMPARATIVE GENOMIC HYBRIDIZATION
-
A molecular cytogenetic method of screening cells for DNA gains and losses at a chromosomal level. Differentially labelled test and reference DNA are hybridized simultaneously to metaphase chromosomes to generate a map of DNA copy number changes.
- ARRAY CGH
-
Similar to conventional comparative genomic hybridization (CGH), but during hybridization, cloned chromosomal DNA fragments (about 200 kb in size) replace the metaphase chromosomes. This method offers greater sensitivity and resolution than conventional CGH in detecting copy number changes.
- HAMARTOMA
-
A focal benign growth that contains an abnormal proportion of a single cell-type or an abnormal mixture of tissue elements that are normally present at that site. Several hereditary cancer predisposition syndromes also feature hamartomas in several tissues, including tuberous sclerosis and Cowden syndrome.
- MATRIGEL
-
The extracellular matrix secreted by the Engelbreth–Holm–Swarm mouse sarcoma cell-line. It contains laminin, collagen IV, nidogen/entactin and proteoglycans, and so resembles the basement membrane.
- ORTHOTOPIC
-
Of identical anatomical location (orthotopic tumour model: transplantation of tumour tissues into an organ from which the tumour originated).
- XENOGRAFT
-
Tissue (for example, human tumour cells) from one animal species grafted onto another animal species (such as subcutaneously into nude mice).
- TRANSDUCTION-ENHANCING AGENT
-
Chemical agents that can increase the efficiency of gene transfer of viral vectors into the host cells.
Rights and permissions
About this article
Cite this article
Wu, XR. Urothelial tumorigenesis: a tale of divergent pathways. Nat Rev Cancer 5, 713–725 (2005). https://doi.org/10.1038/nrc1697
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrc1697
This article is cited by
-
Histomolekulare Klassifikation des Urothelkarzinoms der Harnblase
Die Pathologie (2024)
-
Low expression of ZSCAN4 predicts unfavorable outcome in urothelial carcinoma of upper urinary tract and urinary bladder
World Journal of Surgical Oncology (2023)
-
Tumour microenvironment as a predictive factor for immunotherapy in non-muscle-invasive bladder cancer
Cancer Immunology, Immunotherapy (2023)
-
Rhodamine-Conjugated Anti-Stokes Gold Nanoparticles with Higher ROS Quantum Yield as Theranostic Probe to Arrest Cancer and MDR Bacteria
Applied Biochemistry and Biotechnology (2023)
-
Tenascin-C promotes bladder cancer progression and its action depends on syndecan-4 and involves NF-κB signaling activation
BMC Cancer (2022)