Abstract
Background
The B-MaP-C study aimed to determine alterations to breast cancer (BC) management during the peak transmission period of the UK COVID-19 pandemic and the potential impact of these treatment decisions.
Methods
This was a national cohort study of patients with early BC undergoing multidisciplinary team (MDT)-guided treatment recommendations during the pandemic, designated ‘standard’ or ‘COVID-altered’, in the preoperative, operative and post-operative setting.
Findings
Of 3776 patients (from 64 UK units) in the study, 2246 (59%) had ‘COVID-altered’ management. ‘Bridging’ endocrine therapy was used (n = 951) where theatre capacity was reduced. There was increasing access to COVID-19 low-risk theatres during the study period (59%). In line with national guidance, immediate breast reconstruction was avoided (n = 299). Where adjuvant chemotherapy was omitted (n = 81), the median benefit was only 3% (IQR 2–9%) using ‘NHS Predict’. There was the rapid adoption of new evidence-based hypofractionated radiotherapy (n = 781, from 46 units). Only 14 patients (1%) tested positive for SARS-CoV-2 during their treatment journey.
Conclusions
The majority of ‘COVID-altered’ management decisions were largely in line with pre-COVID evidence-based guidelines, implying that breast cancer survival outcomes are unlikely to be negatively impacted by the pandemic. However, in this study, the potential impact of delays to BC presentation or diagnosis remains unknown.
Similar content being viewed by others
Background
COVID-19 impact in the United Kingdom
The first case of the novel coronavirus SARS-CoV-2 (coronavirus disease 2019, COVID-19) was confirmed in the United Kingdom on January 30, 2020.1 As of August 4, 2020, COVID-19 has resulted in 17,918,582 confirmed cases and 686,703 deaths worldwide since its emergence in December 2019.2 Globally, the COVID-19 pandemic has significantly impacted healthcare delivery, including alterations in cancer care. On 16th March, the UK’s lockdown response was initiated in response to the United Kingdom reaching ‘Alert Level 4’ (transmission high or rising exponentially), with advice against ‘non-essential’ travel, social distancing and guidance on self-isolation.3 On 17th March, NHS England announced that all non-urgent operations in England would be postponed from 15th April to free up 30,000 beds.4 The ‘Alert Level 4’ subsided on 8th May, with the relaxation of the ‘stay at home’ message.
Management of breast cancer in the United Kingdom
There are 55,200 new breast cancer diagnoses per year, which represents 15% of all cancers diagnosed in the United Kingdom.5 Multi-modality treatment, including surgery, radiotherapy (RT) and systemic therapy, involves multiple hospital visits increasing the potential risk of exposure to COVID-19. With current treatments, early breast cancer prognosis is usually excellent.5,6 Compromises to cancer care during the COVID-19 pandemic as a result of rationalisation of resources and prioritisation of individual patient’s cancer versus COVID-19 risks have the potential to impact on survival, as well as the quality of life (QoL), service provision and health economics.
Guidelines for the management of breast cancer during the COVID-19 pandemic
Multidisciplinary UK guidelines, as well as several European and American guidelines, were published early in the alert phase, informing management of breast cancer during the pandemic (Supplementary Tables 1 and 2).7,8,9,10,11,12,13 All aimed to assist rationalisation and prioritisation of delivery of breast services whilst healthcare resources were limited and hospitals were considered a high-infection risk environment. The majority of recommendations did not deviate substantially from pre-COVID National Institute for Health and Care Excellence (NICE) national guidance.6 Guidance emphasised multidisciplinary management, balancing the risk of COVID-19 infection during treatment and the burden of the COVID-19 pandemic on re-structured health services7 to enable the delivery of cancer care whilst safeguarding resources for patients with COVID-19 infection.
When theatre capacity was compromised, guidelines included the use of preoperative, or ‘bridging’, endocrine therapy (ET)14 and priority-driven management based on tumour biology10,13,15 (Supplementary Table 1) with the postponement of non-urgent surgery. Advice included reserving neoadjuvant chemotherapy (NACT)13 for non-operable disease only, careful consideration of the risk/benefit of chemotherapy and streamlined use of adjuvant radiotherapy (RT),16 including potential omission of breast or nodal radiotherapy or use of five-fraction radiotherapy (5F RT). The FAST-Forward trial results, published on April 28, 2020, demonstrated non-inferiority for local recurrence for 5F RT compared to the UK standard of care of 15 fractions (15F) and with improved early and similar late normal tissue toxicity,17 providing evidence for oncologically appropriate RT delivery in a reduced number of visits. There was a move towards creating ‘green’ operating capacity, defined as an operating theatre intended to be COVID-19 free (e.g., theatres geographically separate from patients treated for COVID-19, only doing elective cases with preperative negative SARS-CoV-2 test as a requirement). This is in contrast to a ‘red’ site, defined as an operating theatre delivering emergency surgery in hospitals caring for COVID-19 patients or patients without a preoperative negative COVID test. In the United Kingdom, this involved either restructuring of hospital facilities or sourcing operative capacity in the independent sector.
With the aim of minimising surgical complexity, length of stay and complication risks, and therefore reducing the risk of COVID-19 infection, immediate breast reconstruction (IBR) was suspended, with delayed reconstruction to be offered once services returned to normal. In addition, breast units across the United Kingdom suspended breast screening from March 2020.
Aims and objectives
The aim of the B-MaP-C study was to determine (i) changes to breast cancer management during ‘UK alert level 4’ of the UK COVID-19 pandemic (March 16, 2020 to May 8, 2020),6 (ii) the potential repercussions of these changes to care in terms of oncological impact, quality of life (QoL) and healthcare costs and (iii) the impact of a concurrent COVID-19 diagnosis on patients undergoing treatment for breast cancer.
Methods
A multicentre national cohort study was conducted in which consecutive patients with a diagnosis or early breast cancer undergoing MDT-guided treatment recommendations during the peak of the COVID-19 pandemic were eligible for inclusion.18 Full study information is available on bmapc.org. Patients were identified prospectively by the local participating clinical teams during the UK’s ‘Alert Level 4’ phase of the COVID-19 pandemic (defined as 16th March (the commencement of social distancing recommendations in the United Kingdom) to 8th May [relaxation of the ‘stay at home’ message]).
Data were collected and managed using REDCap™ electronic data capture tools hosted at The University of Manchester,19 in accordance with Caldicott II principles. Each participating unit was required to register the study locally with their hospital audit department and obtain local governance approvals prior to the commencement of data collection. Ethics approval was not required according to the NHS Health Research Authority online decision tool (www.hra-decisiontools.org.uk/research/).18
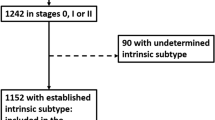
We collected patient demographic data, cancer-specific data and multidisciplinary treatment recommendations in the preoperative, operative and post-operative setting. Patients on NACT prior to the pandemic could enter the study period at the peri- or post-operative multidisciplinary team meeting (MDT-M) (Fig. 1), hence the inclusion of patients having a diagnosis from August 1, 2019. For each management decision, collaborating units determined whether the decision was ‘standard' (i.e., the same as would have been made pre-COVID) or ‘COVID-altered', i.e., not standard management for that unit’s usual practice (even if standard practice for other units). An example would be if a unit’s standard practice is to perform axillary node clearance after positive sentinel node, but during the alert level 4 period, a patient was recommended no further axillary surgery after positive sentinel node.18 Hence, any alterations in management identified were as a direct result of the COVID-19 pandemic, representing treatment out of the ordinary for that collaborating unit. This allowed us to reflect the changes caused by the pandemic, whilst taking into account the background variability of practice across the United Kingdom. Altered management decisions were interrogated in more detail and compared to pre-COVID NICE guidance on breast cancer management6 as well as published COVID-specific guidelines.9,12,13,16,20
Patients may have ‘standard’ treatment at all stages in their management journey or may have ‘COVID-altered’ treatment. This latter group may have ‘COVID-altered’ management in the preoperative, operative or post-operative stage, and may indeed have ‘standard’ management decision at some stage. Overlapping ovals indicate overlapping sub-cohorts. ET endocrine therapy, NACT neoadjuvant chemotherapy, BCS breast-conserving surgery, SM simple mastectomy, Adj. adjuvant, CT chemotherapy, RT radiotherapy, HER2 human epidermal growth factor receptor.
Data analysis
The study was reported in accordance with the STROBE guidelines for observational studies.21 A pre-specified statistical analysis plan was approved by the study steering group. The descriptive analysis examined characteristics of those patients in whom standard management was followed and those with ‘COVID-altered’ management. The subsequent descriptive analysis explored patients’ demographic and clinical characteristics within each altered management scenario. Continuous variables are presented by means (standard deviation, SD) or medians (interquartile range, IQR), categorical variables are presented by frequency (percentage). Calculations for each categorical variable were performed following the exclusion of missing values for this variable only. Non-parametric Mann–Whitney tests were performed to test for differences of medians between groups separately for each continuous and ordinal variable and Chi-squared tests for associations between nominal variables. To understand the national variation in the response to COVID-19, both in terms of MDT-M decisions and logistic arrangements, management decisions for the top 10 recruiting units (as exemplars) were compared. Analyses were computed using Stata MP (version 16). Where pertinent, the benefit of chemotherapy (without taking into account bisphosphonate treatment) using the NHS Predict online tool was calculated.22 Key exemplar healthcare costs (using unit costs from published databases [NHS Reference Costs and Supply Chain]) were compared between routine and ‘COVID-altered’ management to estimate potential financial impacts to the NHS (Supplementary Material).
Data validity
We utilised REDCap’s built-in analysis tools to run tests of data completeness and consistency. In particular, the ‘phased’ data collection offered by the study design allowed us to perform validation checks to ensure consistency of data entry (Supplementary Table 3). Specifically, we calculated the percentage of concordance as the agreement of phases 1 and 2 of the study18 divided by total cases, for each category of ‘COVID-altered’ management.
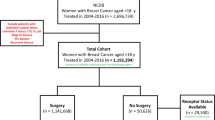
Results
There were 3776 patients included in the study from 64 breast units in the United Kingdom (with rapid data accrual and wide geographical representation from screening and symptomatic units and University Teaching Hospitals and District General Hospitals, Supplementary Fig. 1). Data validity tests showed high agreement in all fields interrogated, ranging from 95 to 99% (Supplementary Table 3). Of the patients included, 1530 (41%) had standard management and 2246 (59%) had ‘COVID-altered’ management at some point within their treatment journey. Patients with the higher-stage disease were statistically more likely to have ‘standard’ management (Table 1). Conversely, screen-detected cancers were more likely to have standard management, which may be a function of fewer screen-detected cancers being treated as the study period progressed (Fig. 2). Patients with ‘COVID-altered’ management had equivalent ER-positive disease (81%) and HER2-positive disease (12%) when compared to contemporary national data.23
Breast cancer management decisions altered due to COVID-19: neoadjuvant treatment
Of the 2216 patients who had MDT-M decisions in the preoperative setting, 252 patients had omitted (n = 160) or incomplete (n = 92) NACT. For those 160 patients where the pandemic resulted in the omission of NACT, the majority (143/156 [92%]) went on to receive ACT.
To allow postponement of surgery, 951 patients had ‘bridging’ ET (defined in the protocol as ‘Patient with hormone receptor-positive cancer having ‘bridging’ endocrine therapy due to a potential delay in surgery’), of which the vast majority (708/862, 82%) were postmenopausal (Table 2). Of patients commenced on ET, 740/774 (96%) were strongly ER-positive (Allred score 7–8), with only 4/774 (<1%) having a score below 5, and 140/900 (15%) assessed pre-operatively as node-positive. Although the primary reason for ‘bridging’ ET is likely due to anticipated reduced theatre capacity, in some, the decision may have been driven by comorbidity and increased risk of COVID-19 mortality.
Surgery
Preoperative imaging assessment was altered in 50 patients, for example with the omission of magnetic resonance imaging to assess disease extent. Of the 957 patients with altered surgical recommendations, 589/957 (62%) had breast-conserving surgery (BCS), 356/957 (37%) had a simple mastectomy and 12/957 (1%) had a mastectomy with IBR. There were 42 patients who had a simple mastectomy when BCS was clinically possible (defined in the protocol as MDT recommendation for simple mastectomy over BCS influenced by potential unavailability of radiotherapy), likely because breast radiotherapy could not be delivered locally. This group had a high number of premenopausal patients (13/40, 33%), with high-grade disease (26/41, 63% grade 3) and disproportionately more ER-negative disease (17/41, 41%) (Table 2), suggesting that oncological considerations impacted these decisions. Thirteen patients had change to standard practice because they had no completion axillary clearance (ANC) following a positive sentinel node, when ANC at that unit would have been offered pre-COVID. There is relative clinical uncertainty around completion ANC in subgroups of patients. For example, based on pre-COVID advice, all 13 patients were eligible for the POSNOC study24 where ANC could have been appropriately omitted. Nine patients also fulfilled Z0011 criteria for the omission of completion axillary clearance.25
The utilisation of IBR has doubled over the last two decades.26 However, in this cohort, there were 299 patients who were not offered IBR, when the usual pre-COVID practice would have included this. These patients were young (median age 50, 61% premenopausal), reflecting a subgroup where IBR would usually be considered a priority. The estimated cost of mastectomy and IBR for these patients would have been £1,636,969, whereas the total cost of mastectomy plus delayed reconstruction is an estimated £3,063,428 (an additional cost of £1,426,459; Supplementary Material).
Adjuvant treatment
Of 1863 patients who had a post-operative MDT-M decision, 81 patients had adjuvant chemotherapy omitted, which would have been offered in the pre-COVID environment, including 13/81 patients with omitted NACT as described above. There were 62/81 patients in whom a decision was made to omit chemotherapy based on clinical grounds (without genomic testing). This group had a median benefit of chemotherapy of 3% (IQR 2–9%) using NHS Predict calculations.22 The majority of patients with omitted chemotherapy were postmenopausal (61/80, 75%), with no/low nodal burden (N0 or N1 = 77/80, 96%) and ER-positive disease (59/81, 73%) with one or more comorbidities (80/81, 99%), implying holistic risk-benefit decision- making (Table 2). Collaborating units were asked to report cases where genomic testing directly influenced MDT-M recommendation to avoid adjuvant chemotherapy (that, following NICE guidance, would not usually have been used pre-COVID). This was the case in 19/81 patients. In addition, extended-indication genomic testing outside of the 2018 NICE guidelines (such as patients with node-positive disease, which was outside of NICE guidance),27 was used in 27 patients, of whom 21 avoided chemotherapy based on genomic test outcome.
Thirteen patients with HER2-positive disease had no adjuvant-targeted (anti-HER2) therapy or chemotherapy when standard management would have included this. The median age of this group was 73 (range 52–84), with low tumour stage (T1 = 5/13, T2 = 7/13), low nodal stage (N0/N1 = 11/13) and largely ER-positive disease (11/13). Four patients with HER2-positive disease received adjuvant anti-HER2 therapy without systemic adjuvant chemotherapy, in accordance with COVID-19 guidance.
There were 96 patients in whom adjuvant radiotherapy was not recommended, whereas pre-COVID local MDT-M practice would have been to recommend radiotherapy. We explored the clinicopathological characteristics of these patients and noted that of these 96, 45 patients (47%) met inclusion criteria for the avoidance of radiotherapy based on NICE guidelines6 or the PRIME2 study.28 In line with the time guidelines for 5F breast and chest wall RT12 and the FAST-Forward publication, 781 patients had adjuvant radiotherapy with 5F where, pre-COVID, 15F would have been administered (Table 2). Of 64 units included in this study, 46 (72%) offered the fast-forward radiotherapy protocol, evidencing the ability to rapidly introduce new clinical practice based on high-quality trial data. As an exemplar of the potential positive health economic impact of changes to management, the cost saving of change to 5 F was investigated. The change from 15F to 5F for these patients is estimated to have saved £1,421,420 (supplementary material). Compared to those having 5F RT, 504 patients receiving 15F were younger (median age 56 years, IQR 49–67 vs 59 years, IQR 53–67, P = 0.006), had larger tumours (mean size 27.6 mm (1·1) vs 20.3 mm (0.6), P = 0.0000), and higher nodal burden (mean number of macrometastatic nodes 2.3 (0.2) vs 0.4 (0.1), P < 0.0001).
Logistic changes to breast surgery during the COVID-19 pandemic
Of 3776 patients, 1778 (47%) had surgery within the study period; 1052 (59%) were in ‘green’ (COVID low-risk) zone operating theatre and 726 (41%) in ‘red’ (COVID high-risk) theatres. There was a move towards increasing access to ‘green’ theatres as the study progressed as units adapted their services in response to the pandemic, from 51 (29%) operations in the first week to 125 (69%) operations in the final week of the study (Fig. 3). The median time to surgery from diagnosis for patients (excluding those on NACT or ET) was 24 days (IQR 16–34), and was similar in both ‘red’ (25 days, IQR 15–33) and ‘green’ (24 days, IQR 16–34) theatres, which is within NHS Breast Screening Programme/NICE pre-COVID targets.
Recommended practice for sentinel lymph node biopsy surgery is with dual localisation using Technicium-99-m isotope and Patent blue dye.29 In 122 cases, sentinel node biopsy was performed with blue dye only. This was more common in ‘green’ theatres that were usually non-NHS independent sector hospitals (117/122, 96%) versus ‘red’ theatres that were usually NHS acute care trusts (5/122, 4%).
Breast cancer management decisions: national variation
To get a sense of the variation in practice across the United Kingdom, we compared changes to normal practice in the ten units contributing the most patient datasets to the study (totalling 37% of the study cohort), with the frequency of ‘standard’ treatment, use of ‘bridging’ ET and use of five-fraction RT as exemplars. Within these ten units, the frequency of standard treatment ranged from 25% to 59%, the frequency of ET from 2% to 35% and of five fractions of RT from 11% to 51% of each hospital’s total patient cohort (Fig. 4a). This may highlight local differences in the ability to access theatre space or to rapidly implement a new evidence-based practice. There was an increase in the number of patients having ‘standard’ treatment and less use of ‘bridging’ ET as the study progressed (Fig. 4b), indicating some recovery in service delivery. In patients commenced on preoperative/’bridging’ ET, 210 patients went on to have surgery by the end of the study. The median length of time of ET for these patients was 22 days (IQR 15–31). The most common reason for proceeding with surgery early was unexpected availability of theatre capacity (53%).
a Variation in management decisions in the top 10 recruiting units, comparing the percentage of patients with (i) standard management (light grey bar), (ii) bridging ET (grey bar) and (iii) 5-fraction RT (black bar). b Trends in management decisions during the study period, by date of diagnosis at weekly intervals.
SARS-CoV-2 testing, outcome and impact on patient journey
There were 1392 patients tested for SARS-CoV-2, the majority in the preoperative setting (1033, 74%). Fourteen patients tested positive (1%). Of 11 patients testing positive before surgery, all were managed at home, without need for hospital admission, with a median time from diagnosis to surgery of 52 days (range 18–168). Those with >90-day delay (n = 2) were temporised with ‘bridging’ NET. There was an increase in preoperative hospital testing during the study period, no doubt, reflecting the increasing availability of SARS-CoV-2 tests nationally (Supplementary Fig. 2). Three patients tested positive post-operatively, of which two had surgery in a red zone.
There was no SARS-CoV-2-related mortality.
Discussion
The COVID-19 pandemic has had unprecedented effects on healthcare provision across the United Kingdom. Early reports from both the United Kingdom and globally have shown that malignancy was a predictor of mortality30,31 and poor outcomes from COVID-19.31,32,33 No previous reports have focused specifically on alterations of care during the pandemic, to early breast cancer patients.34 The major challenges during the pandemic have been to weigh treatment benefit against potential transmission risk of SARS-CoV-2 to patients and healthcare providers, and to administer treatment in healthcare settings where resources and capacity are strained. The rapid publication of guidelines by several organisations7,8,9,10,11,12,13,16 facilitated the implementation of practical evidence-based decisions, as evidenced by the results of this study.
Despite treatment recorded as ‘COVID-altered’ in 2246 (59%) patients as per study definitions,18 the vast majority of patients in this study were treated according to pre-COVID guidelines. Only 439/2246 (19%) patients had a management that was clearly outside the pre-COVID breast cancer NICE guidelines (omission of a reconstruction or premenopausal patients on ‘bridging’ ET), implying that breast cancer oncological outcomes in this study are unlikely to be negatively impacted (although the psychological impact of reconstruction omission is yet to be determined). Where ‘COVID-altered’ management plans had to be instigated, these were mostly within guidelines published during the pandemic. There is likely, however, to be a cohort of women who are yet to present, either symptomatically or through screening, with breast cancer. Their outcomes may be disadvantaged through the late presentation, although that group lies outside the scope of this study.
Where theatre capacity has been an issue, there was increased use of preoperative ET compared to the usual pre-COVID practice,29 largely as ‘bridging’ therapy.35 Indeed, a large number of patients initially placed on ‘bridging’ ET in anticipation of significant surgical delay who have already had surgery, as theatre capacity, particularly in ‘green’ theatres, has increased. In those not receiving any neoadjuvant or bridging treatment (n = 1074), surgery has taken place in a timely manner. This has to be taken in context with the reduction in a number of patients presenting, particularly with screen-detected cancer. It is noteworthy that there were low rates of SARV-CoV-2 infection and no reported COVID-19-related post-operative deaths.
It is evident that some surgical decisions have reflected local resource availability for adjuvant therapies. For example, there was a cohort of patients (n = 42) undergoing simple mastectomy when pre-COVID practice would have been BCS followed by adjuvant RT. These patients were younger, with more aggressive tumour characteristics, and hence this represents, for a short period of time, a decision to prioritise reduction of recurrence risk, whilst there was uncertainty over RT availability. We have identified a large group of patients who have not had IBR when usual practice would have recommended this. UK NICE guidelines recommend all women undergoing a mastectomy be offered IBR.6 However, the COVID-19 pandemic has led to the suspension of IBR in many countries worldwide due to resource, workforce and safety concerns. This may lead to detrimental effects on the aspects of QoL such as body image.
Internationally, standard-of-care chemotherapy treatment regimens have been adapted to minimise the intensity of hospital visits and hospitalisation, and to prevent cancer treatment-induced complications of COVID-19.7,8,9,10,11,13,15,16,20,36 Transferring NACT to the adjuvant setting is oncologically safe,37 but may deprive the patient of the opportunity of downstaging to accommodate BCS, and prevent identification of nonresponders. These nonresponders may potentially be deprived of further adjuvant treatment such as the NICE-approved Trastuzumab emtansine in patients with HER2-positive disease or Capecitabine in patients with triple-negative breast cancer. The majority of patients omitting NACT received adjuvant chemotherapy reflecting the changing scenario during the COVID-19 ‘Alert Level 4’, where initial apprehension for systemic therapy had subsided by the time these patients had completed surgery.
In many units, there has been rapid adoption of the results of the FAST-Forward study, with an almost immediate change to treatment protocols across the country.38 We categorised 5F RT as ‘altered management’ because the start of the study predated the 5-year local control results of the FAST-Forward study, although prepublication national guidelines supported the use of 5F based on 3-year toxicity results of FAST Forward.12 This allowed us to determine the reactiveness of breast cancer services to new evidence and guidance issued during the pandemic. The 5F protocol was advantageous from a service provision perspective, where at the height of the pandemic, the workforce was greatly reduced, as well as from a safety viewpoint, given the reduced number of hospital visits and COVID-19 exposure risk. For those that did not have adjuvant radiotherapy, most were within criteria for planned avoidance of radiotherapy using NICE guidelines6 and PRIME228 criteria. Had research trials been available, these patients may potentially have been recruited into the PRIMETIME study, which had been temporarily closed during the pandemic.
Inevitably, there are some limitations to a study of this nature, particularly one executed in such a short time frame. It is recognised that the data reported in this study have the potential to be subject to reporting bias, data entry error, and indeed, some decisions made early in the COVID-19 ‘alert level 4’ may have been subject to change particularly as the peak of the pandemic subsided. It is also appreciated that the study did not include all units in the United Kingdom, and not all participating units were able to collect data on consecutive patients within the study period, by the study deadline. Nevertheless, this still remains a representative national picture of the impact of the COVID-19 pandemic on breast cancer treatment in the United Kingdom.
Clinical research is a key component of high-quality breast cancer care. In the year 2018/19, over 9000 patients were recruited to breast cancer clinical trials (National Cancer Research Institute Annual Report 18/19). However, the pandemic has resulted in the suspension of many clinical trials, with the redeployment of cancer research staff to allow prioritisation of COVID-19 studies. Across all cancer sites, only 31% of cancer trials continued as planned during the pandemic (National Institute for Health Research (NIHR), personal communication, unpublished data). Although the NIHR has now published a framework for restarting clinical research, recovery of trial recruitment is slow. This has implications for patients in accessing trials and novel treatments, and for researchers to deliver studies to time and target. The extent of this impact on the UK breast cancer clinical research portfolio, however, remains to be elucidated.
Our study has described the extent of changes (and key cost implications) in the management of breast cancer in the United Kingdom during the COVID-19 pandemic on a patient and population-based level, as a response to timely and feasible guidance that was largely followed at a time of national crisis. Appraisal of these changes will guide the evaluation of the impact of the pandemic on immediate patient outcomes and the degree to which breast cancer management has been affected in routine clinical practice. This will assist with planning of service delivery once routine breast cancer management resumes and in the event of a further pandemic. There are significant implications for the COVID-19 ‘recovery’ phase with patients on endocrine therapy requiring cancer resection, and those denied IBR awaiting delayed breast reconstruction. Anticipating the recommencement of breast screening, this delayed (or postponed) activity is likely to overstretch breast surgical services. In the long term, we will have the opportunity to assess the impact of treatment alterations on the rate of disease recurrence and overall patient survival, QoL and the impact of these management decisions on the service and health economics.
Change history
23 June 2021
A Correction to this paper has been published: https://doi.org/10.1038/s41416-021-01465-z
12 April 2021
A Correction to this paper has been published: https://doi.org/10.1038/s41416-021-01378-x
References
Lillie, P. J., Samson, A., Li, A., Adams, K., Capstick, R., Barlow, G. D. et al. Novel coronavirus disease (Covid-19): the first two patients in the UK with person to person transmission. J. Infect. 80, 578–606 (2020).
World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard. https://covid19.who.int/ (2020).
GOV.UK. Prime Minister’s statement on coronavirus (COVID-19): 16 March 2020. https://www.gov.uk/government/speeches/pm-statement-on-coronavirus-16-march-2020 (2020).
Iacobucci, G. Covid-19: all non-urgent elective surgery is suspended for at least three months in England. BMJ 368, m1106 (2020).
Cancer Research UK. Breast cancer statistics. https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/breast-cancer (2020).
National Institute for Health and Care Excellence. Early and locally advanced breast cancer: diagnosis and management (NICE Guideline NG101). https://www.nice.org.uk/guidance/ng12 (2018).
van de Haar, J., Hoes, L. R., Coles, C. E., Seamon, K., Frohling, S., Jager, D. et al. Caring for patients with cancer in the COVID-19 era. Nat. Med. 26, 665–671 (2020).
NHS England. Clinical guide for the management of non- coronavirus patients requiring acute treatment: cancer. https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/specialty-guide-acute- treatment-cancer-23-march-2020.pdf (2020).
National Institute for Health and Care Excellence. COVID-19 rapid guideline: delivery of systemic anticancer treatments. NICE guideline [NG161]. https://www.nice.org.uk/guidance/ng161 (2020).
European Society of Medical Oncology. ESMO management and treatment adapted recommendations in the COVID-19 era: breast cancer. https://www.esmo.org/guidelines/cancer-patient-management-during-the-covid-19-pandemic/breast-cancer-in-the-covid-19-era (2020).
European Society of Breast Imaging. EUSOBI recommendations for breast imaging and cancer diagnosis during and after the COVID-19 pandemic. https://www.eusobi.org/news/recommendations-breast-covid19/ (2020).
Coles, C. E., Aristei, C., Bliss, J., Boersma, L., Brunt, A. M., Chatterjee, S. et al. International guidelines on radiation therapy for breast cancer during the COVID-19 pandemic. Clin. Oncol. (R Coll Radiol) 32, 279–281 (2020).
Association of Breast Surgery. Statement from the association of breast surgery, 15th march 2020. Confidential advice for health professionals. https://associationofbreastsurgery.org.uk/media/252009/abs-statement-150320-v2.pdf (2020).
Dowsett, M., Ellis, M. J., Dixon, J. M., Gluz, O., Robertson, J., Kates, R. et al. Evidence-based guidelines for managing patients with primary ER+ HER2- breast cancer deferred from surgery due to the COVID-19 pandemic. npj Breast Cancer 6, 21 (2020).
Dietz, J. R., Moran, M. S., Isakoff, S. J., Kurtzman, S. H., Willey, S. C., Burstein, H. J. et al. Recommendations for prioritization, treatment, and triage of breast cancer patients during the COVID-19 pandemic. the COVID-19 pandemic breast cancer consortium. Breast Cancer Res. Treat. 181, 487–497 (2020).
Coles, C. Guidelines on radiation therapy for breast cancer during the COVID-19 pandemic. 2020. https://www.rcr.ac.uk/sites/default/files/breast-cancer-treatment-covid19.pdf (2020).
Murray Brunt, A., Haviland, J. S., Wheatley, D. A., Sydenham, M. A., Alhasso, A., Bloomfield, D. J. et al. Hypofractionated breast radiotherapy for 1 week versus 3 weeks (FAST-Forward): 5-year efficacy and late normal tissue effects results from a multicentre, non-inferiority, randomised, phase 3 trial. The Lancet 395, 1613–26 (2020).
Courtney, A., O’Connell, R., Rattay, T., Kim, B., Cutress, R. I., Kirwan, C. C. et al. The B-MaP-C study: breast cancer management pathways during the COVID-19 pandemic. Study protocol. Int. J. Surg. Protoc. 24, 1–5 (2020).
Harris, P. A., Taylor, R., Thielke, R., Payne, J., Gonzalez, N. & Conde, J. G. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 42, 377–381 (2009).
National Institute for Health and Care Excellence. COVID-19 rapid guideline: delivery of radio- therapy. https://www.nice.org.uk/guidance/ng162 (2020).
von Elm, E., Altman, D. G., Egger, M., Pocock, S. J., Gotzsche, P. C., Vandenbroucke, J. P. et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 370, 1453–1457 (2007).
Wishart, G. C., Azzato, E. M., Greenberg, D. C., Rashbass, J., Kearins, O., Lawrence, G. et al. PREDICT: a new UK prognostic model that predicts survival following surgery for invasive breast cancer. Breast Cancer Res. 12, R1 (2010).
National Audit of Breast Cancer in Older Patients. 2020 Annual Report, https://www.nabcop.org.uk/content/uploads/2020/07/NABCOP-2020-Annual-Report-V1_high-res.pdf 2020. Accessed 23 Jun 2020.
Goyal, A. & Dodwell, D. POSNOC: a randomised trial looking at axillary treatment in women with one or two sentinel nodes with macrometastases. Clin. Oncol. 27, 692–695 (2015).
Giuliano, A. E., Ballman, K. V., McCall, L., Beitsch, P. D., Brennan, M. B., Kelemen, P. R. et al. Effect of axillary dissection vs no axillary dissection on 10-year overall survival among women with invasive breast cancer and sentinel node metastasis: the ACOSOG Z0011 (alliance) randomized clinical trial. J. Am. Med. Assoc. 318, 918–926 (2017).
Jeevan, R. Reconstructive utilisation and outcomes following mastectomy surgery in women with breast cancer treated in England. Ann. R Coll Surg. Engl. 102, 110–114 (2020).
National Institute for Health and Care Excellence. Tumour profiling tests to guide adjuvant chemotherapy decisions in early breast cancer. https://www.nice.org.uk/guidance/dg34 (2018).
Kunkler, I. H., Williams, L. J., Jack, W. J., Cameron, D. A., Dixon, J. M. & investigators, P. I. Breast-conserving surgery with or without irradiation in women aged 65 years or older with early breast cancer (PRIME II): a randomised controlled trial. Lancet Oncol. 16, 266–273 (2015).
Public Health England. NHS Breast Screening Programme & Association of Breast Surgery. An audit of screen detected breast cancers for the year of screening April 2017 to March 2018. https://associationofbreastsurgery.org.uk/media/65088/nhsbsp-abs-audit-2017-to-2018.pdf (2020).
Docherty, A. B., Harrison, E. M., Green, C. A., Hardwick, H. E., Pius, R., Norman, L. et al. Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. BMJ 369, m1985 (2020).
Zhang, L., Zhu, F., Xie, L., Wang, C., Wang, J., Chen, R. et al. Clinical characteristics of COVID-19-infected cancer patients: a retrospective case study in three hospitals within Wuhan, China. Ann. Oncol. 31, 894–901 (2020).
CovidSurg, C., Nepogodiev, D. & Bhangu, A. Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br. J. Surg. 107, 1440–1449 (2020).
Lee, L. Y. W., Cazier, J. B., Starkey, T., Turnbull, C. D., Team UKCCMP, Kerr, R et al. COVID-19 mortality in patients with cancer on chemotherapy or other anticancer treatments: a prospective cohort study. Lancet 395, 1919–1926 (2020).
Tasoulis, M. K., Roche, N. & MacNeill, F. Rationalizing breast cancer surgery during the COVID-19 pandemic. Eur. J. Surg. Oncol. 46, 1192–1193 (2020).
Palmieri, C., Cleator, S., Kilburn, L. S., Kim, S. B., Ahn, S. H., Beresford, M. et al. NEOCENT: a randomised feasibility and translational study comparing neoadjuvant endocrine therapy with chemotherapy in ER-rich postmenopausal primary breast cancer. Breast Cancer Res. Treat. 148, 581–590 (2014).
Pardo, R., Algara, M., Montero-Fernández, M. A., Sanz, X., Vernet, M., Rodríguez, N. et al. Diagnosis and locoregional treatment of patients with breast cancer during the COVID-19 pandemic. Revista de Senología y Patología Mamaria 33, 61–67 (2020).
Early Breast Cancer Trialists’ Collaborative Group. Long-term outcomes for neoadjuvant versus adjuvant chemotherapy in early breast cancer: meta-analysis of individual patient data from ten randomised trials. Lancet Oncol. 19, 27–39 (2018).
Lewis, P. J. & Roques, T. W. The response of the UK clinical oncology community to the COVID-19 pandemic. Clin. Oncol. 32, 493–496 (2020).
B-MaP-C Research Collaborative
Amit Agrawal18, John Benson18, Parto Forouhi18, Primeera Wignarajah18, Anu Shrotri19, Arjun Kattakayam19, Jarin Louis Noronha19, Lee Martin19, Mohamed Lafi19, Rob Hardy19, Khalid Amin20, Abdalla Saad Abdalla AL-Zawi21, Mohamed Elamass21, Ali Salih21, Firas Eddin Bachir Alkistawi21, Anna Heeney22, Arnold D. K. Hill22, Colm Power22, Michael J. Allen22, Ashok Chouhan23, Rathi Rathinaezhil23, Samy Shaheed23, Charles Zammit23, Gillian Clayton24, Sascha Dua24, Simon Smith24, Tasha Gandamihardja24, Chloe Williams25, Donna Egbeare25, Eleri Davies25, Helen M. Sweetland25, Sharat Chopra25, Sumit Goyal25, Dalia Elfadl26, Dheer Singh Rana26, Eliana Kalakouti26, Musa Barkeji26, Rajiv Vashisht26, Ralia Bunza26, Saung Hnin Phyu26, Ciaran Hollywood27, Iman Azmy27, Julia Massey27, Anita Hargreaves28, Claudia Harding-Mackean28, Jane Ooi28, Joanna Seward28, Helen Mathers29, Norah Scally29, Reem Salman29, Hyunjin Shin30, Jane Turner30, Lubna Noor30, Sanjay Joshi30, Sarah Horne30, Wail Al Sarakbi30, Peter Liptay- Wagner31, Rosamond Jacklin31, Sankaran Chandrasekharan31, Simon Marsh31, Sunita Saha32, Christopher Wilson33, Claire Louise Rutherford33, Julie Doughty33, Laszlo Romics33, Sheila Stallard33, Anushka Chaudhry34, Jennifer Peck34, Nathan Coombs34, Samantha K. Williams34, Simon Hawkins34, Ashutosh Kothari35, Hisham Hamed35, Urvashi Jain35, Ian Daltrey36, Nick Abbott36, Russell Mullen36, Dorin Dumitru37, Eiman Khalifa37, Masuma Sarker37, M. Bilal Elahi37, Raouef Ahmed Bichoo37, Anzors Gvaramadze38, Dinesh Thekkinkattil38, Jibril Jibril38, Demetrios Hadjiminas39, Edward R. C. St John39, Henry Douglas Robb39, Katy Hogben39, Nur Amalina Che Bakri39, Paul Thiruchelvam39, Georgios Exarchos39, Ragheed Al-Mufti39, Caroline Mortimer40, Evangelos Mallidis40, Georgios Karagiannidis40, Hussein Tuffaha40, Inga Peerlink40, Rajive Nair41, Dinesh Thekkinkattil41, Lydia Prusty41, Anzors Gvaramadze41, Jibril Jibril41, Amtul Sami41, Alex Knight42, Duraisamy Ravichandran42, Katharine Kirkpatrick42, Ruth James42, Deepika Akolekar43, Disha Mehta43, Ellora Barua43, Hannah Knowles43, Haresh Devalia43, Karina Cox43, Mohsin Dani43, Ritchie Chalmers43, Anjana Satpathy44, Edel Quinn44, Gerard Byrne44, James Harvey44, John Murphy44, Lyndsey Highton44, Mohammad Amir Sharif44, Nicola Barnes44, Nikitas Dimopoulos44, Richard Johnson44, Sumohan Chatterjee44, Hiba Fatayer44, Vinod Mathen44, Amanda Taylor45, Rachel Soulsby45, Adam Walsh46, Amanda Thorne46, Jasper Gill46, Louise Merker46, Adam Critchley47, Andrew Pieri47, Henry Cain47, Jane Ralph47, Loraine Kalra47, Robert Thomas47, Ian Young48, Lucy R. Khan49, Beatrix Elsberger50, Elizabeth Smyth50, Gordon Urquhart50, Mairi Fuller50, Yazan Masannat50, Ada Chrysafi51, Muhammad Salman51, El-Rasheed Abdalla51, Katalin Zechmeister52, Maged Hussien52, Mina M. G. Youssef52, Angeline Tanhueco52, Reginald Salvador53, Sharon Wallace53, Simon Pain53, Ajay Sahu54, Alice Chambers54, Alice Moody54, Isabella Dash54, James Cook54, Jeremy Batt54, Michelle Mullan54, Mike Shere54, Nicholas Gallegos54, Rachel Ainsworth54, Sasi Govindarajulu54, Shelley Potter54, Zenon Rayter54, Kate E. Williams55, Maria Bramley55, Mohammed Absar55, Nabila Nasir55, Rami Tabbakh55, Bernadette Pereira56, Jasdeep Gahir56, Karen Bosch56, Oladapo Fafemi56, Nader Touqan57, Georgette Oni58, Hazem Khout58, Kristjan Asgeirsson58, Lisa Whisker58, Rachel Xue Ning Lee58, Robert Macmillan58, Stephen McCulley58, Tuabin Rasheed58, Asha Adwani59, Ashvina Segaran59, David Dodwell59, Dennis Remoundos59, Gael MacLean59, Giulio Cuffolo59, Michael Douek59, Pankaj Roy59, Toral Gathani59, Mohammed Absar60, Erum Najeeb61, Claudiu Simonca62, Maria Verroiotou62, Sa’ed Ramzi62, Stephanie C. Jenkins62, Vallipuran Gopalan62, Sarah Barker63, Ciara McGoldrick64, Gareth W. Irwin64, Peter Mallon64, Samantha A. Sloan64, Abbas Imran65, Giuseppina Mondani65, Iain Brown65, Imran Abbas65, Mona Sulieman65, Philip Drew65, Polly King65, Rachel Elizabeth English65, Anita Sharma66, Charlotte Ives66, Douglas Ferguson66, George Boundouki66, James Bentley66, Jenny Banks66, Julie Dunn66, Rachel Tillett66, Sisse Olsen66, Anne Tansley67, Emma de Sousa67, Geraldine Mitchell67, Ian Whitehead67, Julia Henderson67, Matthew Rowland67, Mysore Chandrashekar67, Raja Eid67, Elizabeth Clayton68, Farrokh Pakzad68, Jonathan D. Horsnell68, Matthew Hague68, Polly Partlett68, Tracey Irvine68, Charlotte Kallaway69, Katherine Fairhurst69, Christiana Laban70, Jamie McIntosh70, Nicola Laurence70, Richard Sutton70, Anup Sharma71, Dibyesh Banerjee71, Nadine Betambeau71, Sabrina Bezzaa71, Sonia Bathla72, Atanu Ray72, Leena Chagla72Sonia BathlaTamara Kiernan72, Brian Hogan73, Channegowda Navin73, Emma Macinnes73, Philip Turton73, Raj Achuthan73, Venla Kantola73, Shireen Mckenzie73, Helen Dent74, Caroline Pogson74, Shamaela Waheed74, Tania S. de Silva74, Usama Suleiman74, Lucie Jones75, Ruvinder Athwal75, Simon Harries75, Catherine Krzyzanowska76, Abeera Abbas77, Anna R. Hurley77, Gerald Gui77, Jennifer E. Rusby77, Katherine Krupa77, Kathryn E. Harborough77, Nicola Roche77, Peter A. Barry77, Rebekah Law77, William H. Allum77, Cheryl Lobo78, Eleni Ntakomyti78, Joanna Franks78, Massimiliano Cariati78, Neill Patani78, Noyko Stanilov78, Petros Charalampoudis78, Zarghuna Taraki78, Kat McEvoy79, Mohamed Razick Sait79, Stuart Robertson79, Bashar Zeidan80, David Rew80, Fayyaz Mazari80, Louise Alder80, Vasileios Sakellariou80, Ahmed Hamad81, Amit Goyal81, Amtul Carmichael81, Carol-Ann Courtney81, David Mark Sibbering81, Emanuele Garreffa81, Kwok-Leung Cheung81, Susan Williams-Jones81, Yasmin Wahedna81, Aonghus Ansari82, Frances Kenny82, Kalliope Valassiadou82, Kelly Lambert82, Jaroslaw Krupa82, Mini V. Sardar82, Monika Kaushik82, Sheila Shokuhi82, Simon Pilgrm82, Walid Sasi82, Penelope McManus83, Rishikesh Parmeshwar83, Santosh Somasundaram83, Manoj Gowda84, Sadaf Jafferbhoy84, Sankaran Narayanan84, Sekhar Marla84, Soni Soumian84, Ngee-Ming Goh85, Jamie Vatish86, Tin Aung Sein86, Ennio Agabiti87, Joseph Maalo87, Kelvin Chong87, Lee-Min Lai87, Mohamed Elkorety87, Sherif Monib87, Simon Thomson87, Youhana Mikhael87, Bahar Mirshekar-Syahkal88, Jane Aitken88, Mina Girgis88, Dibendu Betal89, Fabio Rapisarda89, Lorna Cook89, Olubunmi Odofin89, Riccardo Bonomi89, Stacy Wardle89, Wendy Sotheran89, Irene Athanasiou90, Jonathan Lund91, Maria Callaghan91, Rajaram Burrah91, Raman Vinayagam91, Karen James91, Shabbir Poonawala91, Brian Isgar92, Pilar M3atey92, Senthurun Mylvaganam92, Carl Podesta92, Tapan Sircar92, Fathi Salem92, Zaid Al-Ishaq92
Author information
Authors and Affiliations
Consortia
Contributions
R.V.D. conceived the study. R.V.D., B.K., R.I.C., A.G. and C.C.K. designed the pilot study. R.V.D., B.K., A.C., R.O.C. and T.R. designed and trialled the pilot data collection forms. R.V.D., B.K., A.C., R.O.C., T.R., V.P.T., J.J.K., E.M.C., P.F., N.S., C.W.J.C., K.H., S.A.M., D.R.L., R.V., S.P., C.H., E.C., C.E.C., R.I.C., A.G. and C.C.K. contributed to the final study design and finalised data collection forms. A.C., R.V.D., R.O.C. and T.R. designed the study website, and coordinated collaborator recruitment and provided collaborator support. R.V.D., B.K., K.H., P.F., N.S., C.W.J.C., R.V., S.P., S.A.M., D.R.L., C.H., E.C., C.E.C., R.I.C., A.G. and C.C.K. provided clinical leadership and promoted unit participation and data collection. V.P.T., J.J.K. and E.M.C. provided methodological support. R.V.D., V.P.T., J.J.K. and E.M.C. drafted the statistical analysis plan and analysed the data. All authors contributed to data interpretation. R.V.D. led the study and wrote the first draft of the paper, with support from B.K., J.J.K., K.H., S.A.M., R.I.C., A.G. and C.C.K. All authors reviewed and critically revised the paper and approved it before submission.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Ethics approval was not required according to the NHS Health Research Authority online decision tool (www.hra-decisiontools.org.uk/research/).
Data availability
Data supporting the results reported in the paper cannot be found on publicly available databases. The data have been uploaded by collaborators onto a RedCap database, and individual units have access to their own data, but not the overall national data.
Competing interests
The authors declare no competing interests. R.V.D., B.K., A.C., R.O’C., V.P.T., R.V., J.J.K., P.F., N.S., C.W.J.C., K.H., S.P., A.G., S.A.M., E.M.C., D.R.L. and C.H. have nothing to declare. Dr Tim Rattay (T.R.) is currently an NIHR Clinical Lecturer. Charlotte E Coles (C.E.C.) is supported by the National Institute Health Research Cambridge Biomedical Research Centre. Ramsey I Cutress (R.I.C.) has equipment provided by Seca to analyse body composition to University Hospital Southampton as part of an NIHR model industry collaborative agreement (MiCA). This equipment is used in an Academic Investigator-led charity-funded study of which Ramsey Cutress is CI. Ellen Copson (E.C.) declares honoraria from Roche, Pfizer, Astra-Zeneca, Lilly, Nanostring and expert panel work for World Cancer Research Fund. Cliona C. Kirwan (C.C.K.) is Royal College of Surgeons/University of Manchester Professor of Surgical trials funded by a Royal College of Surgeons of England/Masonic Charitable Foundation professorship.
Funding information
There is no dedicated funding for this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The matadata of this article had to be corrected due to an error in typesetting
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dave, R.V., Kim, B., Courtney, A. et al. Breast cancer management pathways during the COVID-19 pandemic: outcomes from the UK ‘Alert Level 4’ phase of the B-MaP-C study. Br J Cancer 124, 1785–1794 (2021). https://doi.org/10.1038/s41416-020-01234-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-020-01234-4
This article is cited by
-
Cancer management during the COVID-19 world pandemic
Cancer Immunology, Immunotherapy (2023)
-
Bridging pre-surgical endocrine therapy for breast cancer during the COVID-19 pandemic: outcomes from the B-MaP-C study
Breast Cancer Research and Treatment (2023)
-
Raman spectroscopy: current applications in breast cancer diagnosis, challenges and future prospects
British Journal of Cancer (2022)
-
Highly specialized Breast Centers did not experience delay of care during COVID-19 pandemic in Italy: the Senonetwork experience
Breast Cancer Research and Treatment (2022)